ASTM E1327-07(2012)e1
(Test Method)Standard Test Method for Evaluation of Antimicrobial Handwash Formulations by Utilizing Fingernail Regions
Standard Test Method for Evaluation of Antimicrobial Handwash Formulations by Utilizing Fingernail Regions
SIGNIFICANCE AND USE
4.1 The procedure should be used to test the degerming effectiveness of antimicrobial hand washing products used by health care personnel that are intended for frequent use, and that are intended to reduce the level of contamination acquired through contact with contaminated objects or people.
4.2 Performance of these procedures requires the knowledge of regulations pertaining to the protection of human subjects (Ref 1).3
SCOPE
1.1 This test method can be used to determine the effectiveness of antimicrobial handwashing agents (including handrubs) in the reduction of transient bacterial flora with particular emphasis on the fingernail region.
1.2 A knowledge of microbiological techniques is required for these procedures.
1.3 This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety and health practices and determine the applicability of regulatory limitations prior to use. For more specific hazard statements, see 7.5.
General Information
Relations
Standards Content (Sample)
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Contact ASTM International (www.astm.org) for the latest information
´1
Designation: E1327 − 07 (Reapproved 2012)
Standard Test Method for
Evaluation of Antimicrobial Handwash Formulations by
Utilizing Fingernail Regions
This standard is issued under the fixed designation E1327; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (´) indicates an editorial change since the last revision or reapproval.
ε NOTE—Editorial changes were made throughout the document in November 2012.
1. Scope refrain from using topical antimicrobials (such as deodorant
soaps) before participating in the study.All subjects wash their
1.1 This test method can be used to determine the effective-
hands with a nonantimicrobial hand soap prior to testing to
nessofantimicrobialhandwashingagents(includinghandrubs)
remove any residual hand lotions and to lower the numbers of
in the reduction of transient bacterial flora with particular
resident skin flora. Activity of products is measured by
emphasis on the fingernail region.
comparing the numbers of marker bacteria recovered from
1.2 A knowledge of microbiological techniques is required
artificially contaminated fingernail regions after use of the
for these procedures.
handwashing formulations to the numbers recovered from the
1.3 This standard does not purport to address all of the
artificially contaminated but unwashed fingernail regions.
safety concerns, if any, associated with its use. It is the Broth cultures of Serratia marcescens (a red pigmented bac-
responsibility of the user of this standard to establish appro-
terial species) and Escherichia coli (which produces fluores-
priate safety and health practices and determine the applica- cent colonies on a special agar medium) are used as test
bility of regulatory limitations prior to use. For more specific
bacteria. A spore suspension of Bacillus subtilis may be
hazard statements, see 7.5. utilized to study (1) degree of physical removal by handwash-
ing techniques, and (2) the recovery and precision aspects of
2. Referenced Documents
the test method.
2.1 ASTM Standards:
4. Significance and Use
E1054 Test Methods for Evaluation of Inactivators of Anti-
4.1 The procedure should be used to test the degerming
microbial Agents
effectiveness of antimicrobial hand washing products used by
E2276 Test Method for Determining the Bacteria-
health care personnel that are intended for frequent use, and
Eliminating Effectiveness of Hygienic Handwash and
that are intended to reduce the level of contamination acquired
Handrub Agents Using the Fingerpads of Adults
through contact with contaminated objects or people.
E1838 Test Method for Determining the Virus-Eliminating
Effectiveness of Hygienic Handwash and HandrubAgents
4.2 Performance of these procedures requires the knowl-
Using the Fingerpads of Adults
edge of regulations pertaining to the protection of human
subjects (Ref 1).
3. Summary of Test Method
5. Apparatus
3.1 This test method, involving an improved method of
recovering bacteria from hands, is used to study the effects of
5.1 Colony Counter—Any of several types may be used, for
antimicrobial handwashes including health care personnel example, Quebec Colony Counter.
handwash products. The group of volunteer panelists need not
5.2 Incubators—One incubator capable of maintaining a
temperatureof25 62°C(thistemperatureisrequiredtoensure
pigment production of Serratia); a second incubator capable of
This test method is under the jurisdiction of ASTM Committee E35 on
maintaining 37 6 2°C used for E. coli and B. subtilis
Pesticides, Antimicrobials, and Alternative Control Agents and is the direct
responsibility of Subcommittee E35.15 on Antimicrobial Agents.
incubation is acceptable.
Current edition approved Oct. 1, 2012. Published November 2012. Originally
5.3 Water Bath—Capable of maintaining temperature of 80
approved in 1990. Last previous edition approved in 2007 as E1327 – 07. DOI:
10.1520/E1327-07R12E01.
6 2°C for heat shocking of B. subtilis spores is needed.
For referenced ASTM standards, visit the ASTM website, www.astm.org, or
contact ASTM Customer Service at service@astm.org. For Annual Book of ASTM
Standards volume information, refer to the standard’s Document Summary page on The boldface numbers in parentheses refer to a list of references at the end of
the ASTM website. this standard.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959. United States
´1
E1327 − 07 (2012)
5.4 Sterilizer—Any suitable steam sterilizer capable of pro- 6.8 Test Formulations—Directions for use of test formula-
ducing the conditions of sterilization is acceptable. tion should be included if available. If these are not available,
liquid antimicrobial soap formulations are tested by same
5.5 Timer—Any stop-watch that can be read in minutes and
routine as the nonantimicrobial control (10.5); alcoholic lotion
seconds is required.
type formulations are rubbed to dryness and then sampled for
5.6 Handwashing Sink—A sink of sufficient size to permit
survivors (10.7).
panelists to wash without touching hands to sink surface or
6.9 Nonantimicrobial Control Soap, a liquid castile soap or
other panelists is needed.
other liquid soap containing no antimicrobials.
5.6.1 Water Faucet(s), to be located above the sink at a
height that permits the hands to be held higher than the elbow 6.10 Broth—Tryptic soy broth or equivalent is required.
during the washing procedure.
7. Test Organisms
5.6.2 Tap Water Temperature Regulator and Temperature
Monitor, to monitor and regulate water temperature of 40 6
7.1 Serratia marcescens AmericanType Culture Collection,
2°C.
ATCC No. 14756 is to be used as a marker organism. This is
a strain having stable pigmentation. Grow in tryptic soy broth
5.7 Quad Petri plates, 100 by 15 mm, plastic, sterile,
at 25 6 2°C.
disposable.
7.2 Escherichia coli, ATCC No. 11229 is used as another
5.8 Small Petri Plates, 60 by 15 mm, glass.
Gram-negative marker organism. Grow in tryptic soy broth at
5.9 Large Petri Plates, 150 by 15 mm, glass.
35 6 2°C.
5.10 Tooth Brushes:
7.3 Bacillus subtilis, ATCC No. 19659. Grow in tryptic soy
5.10.1 Young Size.
broth at 35 6 2°C.
5.10.2 Battery Operated.
7.4 Preparation of Spore Suspension—Inoculate each sur-
5.11 Ultraviolet Lamp, having separate short wave and long
faceoftwotrypticsoyagarplates(30mLagarin150-mmpetri
wave bulbs.
plates) with 1 mL of B. subtilis tryptic soy broth culture.
5.12 Germicidal Lamp Monitor Strips.
Spread over the entire surface of the agar. Incubate for 5 to 10
days at 35 6 2°C. Suspend the growth in 20 mL of 0.1 %
5.13 Inoculating Loops or Needles, sterile.
tryptone water by rubbing the agar surface with a sterile
5.14 Plate Spreaders or Hockey Sticks, sterile.
rubber policeman. Add ethanol to the suspension to a final
concentration of 80 % (wt/wt) and store in a refrigerator.
6. Reagents and Materials
7.5 Other bacteria containing adequate markers to enable
6.1 Bacteriological Pipettes, 10.0 mL, sterile.
distinction from normal flora and of known safety may also be
6.2 Pipettors and Pipette Tips, Eppendorf, MLA or similar
used for testing purposes. (Warning—The application of
types.
microorganisms to the skin may involve a health risk. Prior to
applying S. marcescens or other bacteria to the skin, the
6.3 Disposable Analyzer Cups, 2 mL, plastic, not sterile.
antibiotic susceptibility profile of the strain should be deter-
6.4 Sampling Solution—Dissolve 0.4 g KH PO , 10.1 g
2 4
mined. If the Serratia strain is not sensitive to Gentamicin, it
Na PO and 1.0 g isooctylphenoxypolyethoxyethanol in1L
2 4
should not be used. If an infection occurs, the antibiotic
distilled water. Adjust pH to 7.8 with 0.1 N HCl or 0.1 N
susceptibility profile should be made available to an attending
NaOH. Dispense in 100 mL-volumes and sterile for 20 min at
clinician. Following the panelist’s contamination and testing
121°C.
fortheday,thepanelist’shandsshouldbedecontaminatedwith
6.5 Dilution Fluid—The sampling fluid may be used for
a 70-% ethanol solution. Care should be taken to decontami-
dilutions or use Butterfields sterile phosphate buffered water
nate around the fingernail regions.)
(2) adjusted to pH 7.2 with suitable inactivator for the
7.6 Preparation of Marker Culture Suspension—Inoculate a
antimicrobial. Adjust pH with 0.1 N HCl or 0.1 N NaOH (see
10-mLtryptic soy broth tube with each of the test bacteria and
Practices E1054).
incubateeachtubeatthetemperatureindicatedtoyieldinocula
8 9
6.6 Agar, Tryptic soy agar or equivalent. Include the appro-
of 10 –10 CFU/mL.When studying mixed inocula, mix equal
priate inactivator if needed.
volumes of the cultures into a sterile test tube; an equivalent
volume of B. subtilis spore suspension (that is prepared by
6.7 Agar with MUG—Tryptic soy agar with 60 to 80 µg/mL
centrifuging the alcoholic suspension and resuspending cells in
4-methylumbelliferyl-β-D-glucuronide (MUG) is required.
water) may be added for bacterial physical removal determi-
nations.Keepmixedsuspensiononiceduringtheday’stesting.
Presterilized disposable quad plastic petri plates, the two sizes of glass petri
plates and other equipment are available from most local laboratory supply houses.
5 6
The sole source of supply of the apparatus (Triton X-100) known to the The sole source of supply of the Bacto Tryptone (Difco) water known to the
committee at this time is Rohm and Haas Co., Philadelphia, PA. If you are aware of committee at this time is Difco Laboratories, Detroit, MI. If you are aware of
alternative suppliers, please provide this information to ASTM International alternative suppliers, please provide this information to ASTM International
Headquarters.Your comments will receive careful consideration at a meeting of the Headquarters.Your comments will receive careful consideration at a meeting of the
1 1
responsible technical committee, which you may attend. responsible technical committee, which you may attend.
´1
E1327 − 07 (2012)
8. Panelists 10.3 Place 0.02 mL of marker culture suspension on the
region surrounding the cuticle and under the fingernails of
8.1 Recruit a sufficient number of healthy adult human
three fingers of the left hand of a volunteer. The volunteer then
volunteers who have no clinical evidence of dermatoses, open
holdsthehandinfrontofanelectricfanfor5minforcomplete
wounds, hangnails, or other skin disorders. The number of
drying of the suspension.
people needed for a trial is dependent on the number of
treatments within a study.
10.4 For unwashed hand determinations, proceed directly to
10.8.
8.2 Volunteers are asked to maintain their normal use of
soaps, shampoos, and so forth. They are asked to refrain from
10.5 When testing nonantimicrobial soap (controls), wet
the use of acids, bases, solvents on the hands during the test
both hands under flowing warm tap water (40 6 2°C).Add 2.5
period. Gloves should be provided for use where exposure to
to 3.0 mL of the liquid soap to hands, rub hands together in
these agents is unavoidable.
normal washing manner for 15 s (no additional water), then
rinse under the flowing water for 15 s to remove suds. Do not
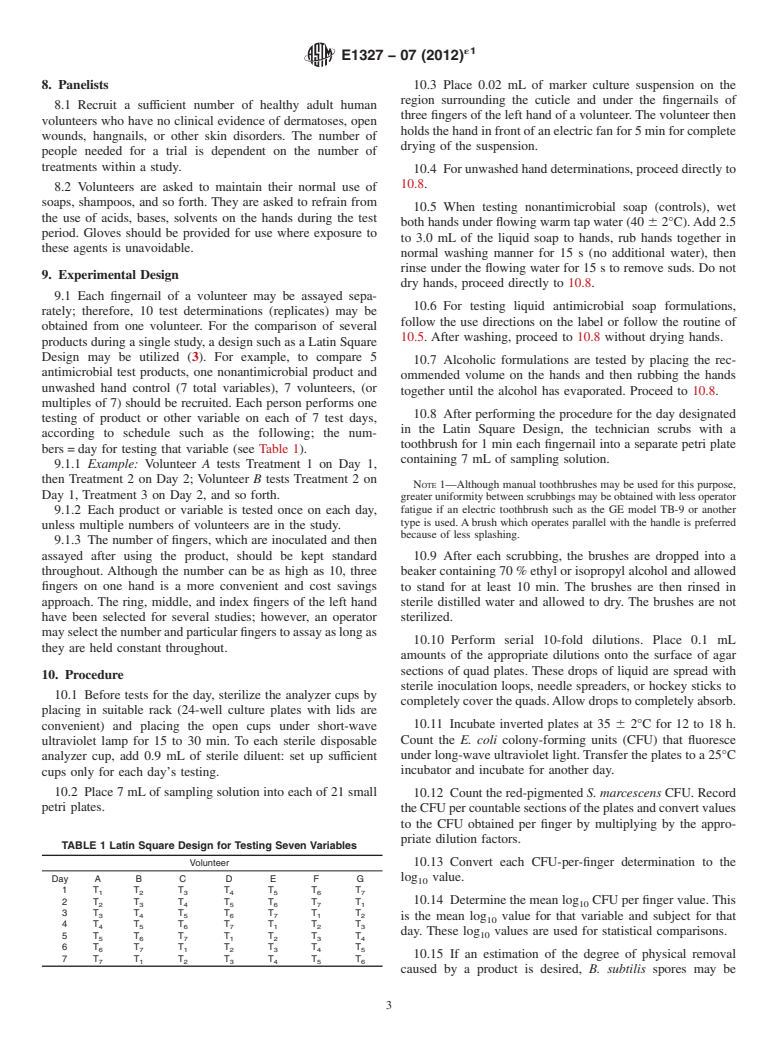
9. Experimental Design
dry hands, proceed directly to 10.8.
9.1 Each fingernail of a volunteer may be assayed sepa-
10.6 For testing liquid antimicrobial soap formulations,
rately; therefore, 10 test determinations (replicates) may be
follow the use directions on the label or follow the routine of
obtained from one volunteer. For the comparison of several
10.5. After washing, proceed to 10.8 without drying hands.
products during a single study, a design such as a Latin Square
Design may be utilized (3). For example, to compare 5
10.7 Alcoholic formulations are tested by placing the rec-
antimicrobial test products, one nonantimicrobial product and
ommended volume on the hands and then rubbing the hands
unwashed hand control (7 total variables), 7 volunteers, (or
together until the alcohol has evaporated. Proceed to 10.8.
multiples of 7) should be recruited. Each person performs one
10.8 After performing the procedure for the day designated
testing of product or other variable on each of 7 test days,
in the Latin Square Design, the technician scrubs with a
according to schedule such as the following; the num-
toothbrush for 1 min each fingernail into a separate petri plate
bers = day for testing that variable (see Table 1).
containing 7 mL of sampling solution.
9.1.1 Example: Volunteer A tests Treatment 1 on Day 1,
then Treatment 2 on Day 2; Volunteer B tests Treatment 2 on
NOTE 1—Although manual toothbrushes may be used for this purpose,
Day 1, Treatment 3 on Day 2, and so forth.
greater uniformity between scrubbings may be obtained with less operator
9.1.2 Each product or variable is tested once on each day, fatigue if an electric toothbrush such as the GE model TB-9 or another
type is used. A brush which operates parallel with the handle is preferred
unless multiple numbers of volunteers are in the study.
because of less splashing.
9.1.3 The number of fingers, which are inoculated and then
assayed after using the product, should be kept standard 10.9 After each scrubbing, the brushes are dropped into a
throughout. Although the number can be as high as 10, three beaker containing 70 % ethyl or isopropyl alcohol and allowed
fingers on one hand is a more convenient and cost savings to stand for at least 10 min. The brushes are then rinsed in
approach. The ring, middle, and index fingers of the left hand sterile distilled water and allowed to dry. The brushes are not
have been selected for several studies; however, an operator sterilized.
mayselectthenumberandparticularfingerstoassayaslongas
10.10 Perform serial 10-fold dilutions. Place 0.1 mL
they are held constant throughout.
amounts of the appropriate dilutions onto the surface of agar
sections of quad plates. These drops of liquid are spread with
10. Procedure
sterile inoculation loops, needle spreaders, or hockey sticks to
10.1 Before tests for the day, sterilize the analyzer cups by
completelycoverthequads.Allowdropstocompletelyabsorb.
placing in suitable rack (24-well culture plates with lids are
10.11 Incubate inverted plates at 35 6 2°C for 12 to 18 h.
convenient) and placing the open cups under short-wave
Count the E. coli colony-forming units (CFU) that fluoresce
ultraviolet lamp for 15 to 30 min. To each sterile disposable
under long-wave ultraviolet light.Transfer the plates to a 25°C
analyzer cup, add 0.9 mL of sterile diluent: set up sufficient
incubator and incubate for another day.
cups only for each day’s testing.
10.2 Place 7 mL
...







Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.