ASTM E2784-10
(Test Method)Standard Test Method for Evaluation of the Effectiveness of Handwash Formulations Using the Paper Towel (Palmar) Method of Hand Contamination
Standard Test Method for Evaluation of the Effectiveness of Handwash Formulations Using the Paper Towel (Palmar) Method of Hand Contamination
SIGNIFICANCE AND USE
This procedure has been designed to evaluate handwash products using a palmar surface only contamination method. This method is an alternative contamination procedure to that listed in Test Method E1174. The current contamination procedure in Test Method E1174 describes a standardized procedure for contaminating the entire hand, palmar surface and back, directly using a marker organism. The contamination procedure in Test Method E1174 does not necessarily represent real world hand contamination. During routine activities it is only the palmar surface, comprising palms, fingers, and finger pads of the hands that becomes contaminated by contact with transient microorganisms. These microorganisms can then be transferred to food or objects. Methods to measure the amount of microorganisms transferred to food or objects can be found in Fischler et al and Fuls et al and will be developed into a future ASTM standard.
SCOPE
1.1 This test method covers the determination of the effectiveness of antimicrobial handwashing agents for the reduction of transient microbial flora when used in a handwashing procedure.
1.2 A knowledge of microbiological techniques is required for these procedures.
1.3 This test method may be used to evaluate topical antimicrobial handwash formulations.
1.4 Performance of this procedure requires the knowledge of regulations pertaining to the protection of human subjects.
1.5 In this test method, SI units are used for all applications, except for distance in which case inches are used and SI units follow in parentheses.
1.6 This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety and health practices and determine the applicability of regulatory limitations prior to use. For more specific precautionary statements see 8.5.
General Information
Relations
Standards Content (Sample)
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Contact ASTM International (www.astm.org) for the latest information
Designation: E2784 − 10
StandardTest Method for
Evaluation of the Effectiveness of Handwash Formulations
Using the Paper Towel (Palmar) Method of Hand
Contamination
This standard is issued under the fixed designation E2784; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision.Anumber in parentheses indicates the year of last reapproval.A
superscript epsilon (´) indicates an editorial change since the last revision or reapproval.
1. Scope 2.2 Other Standards:
AATCC Test Method 147Antibacterial Assessment of Tex-
1.1 This test method covers the determination of the effec-
tile Materials: Parallel Streak Method
tivenessofantimicrobialhandwashingagentsforthereduction
of transient microbial flora when used in a handwashing
3. Terminology
procedure.
3.1 Definitions:
3.1.1 active ingredient, n—a substance added to a formula-
1.2 A knowledge of microbiological techniques is required
tion specifically for the inhibition or inactivation of microor-
for these procedures.
ganisms.
1.3 This test method may be used to evaluate topical
3.1.2 cleansing wash, n—a procedure intended to remove
antimicrobial handwash formulations.
soilorresidue.Thismayalsobereferredtoasacosmeticwash.
1.4 Performance of this procedure requires the knowledge
3.1.3 healthcare personnel handwash, n—a cleanser or
of regulations pertaining to the protection of human subjects.
waterless agent intended to reduce transient bacteria on the
hands.
1.5 Inthistestmethod,SIunitsareusedforallapplications,
except for distance in which case inches are used and SI units 3.1.4 neutralization, n—the process for inactivating or
follow in parentheses. quenching the activity of a microbiocide. Often achieved
through chemical or physical means (for example, filtration or
1.6 This standard does not purport to address all of the
dilution).
safety concerns, if any, associated with its use. It is the
3.1.5 resident microbial skin flora, n—microorganisms that
responsibility of the user of this standard to establish appro-
survive and multiply on the skin, forming a stable population.
priate safety and health practices and determine the applica-
bility of regulatory limitations prior to use. For more specific 3.1.6 test material, n—a formulation which incorporates
precautionary statements see 8.5. antimicrobial ingredient(s).
3.1.7 test organism, n—anappliedinoculumofanorganism
2. Referenced Documents
that has characteristics which allow it to be readily identified.
3 The test organism is used to simulate a transient topical
2.1 ASTM Standards:
microbial contaminant. It may also be referred to as a marker
E1054Test Methods for Evaluation of Inactivators of Anti-
organism, bacterial simulant, or bacterial contaminant.
microbial Agents
3.1.8 transient microbial skin flora, n—microorganismsthat
E1174Test Method for Evaluation of the Effectiveness of
contaminate the skin but do not normally form a stable
Health Care Personnel Handwash Formulations
population.
4. Summary of Test Method
This test method is under the jurisdiction of ASTM Committee E35 on
4.1 This test method is conducted on a group of volunteer
Pesticides, Antimicrobials, and Alternative Control Agents and is the direct
responsibility of Subcommittee E35.15 on Antimicrobial Agents.
subjects who have refrained from using topical antimicrobial
Current edition approved Oct. 1, 2010. Published November 2010. DOI:
formulations for at least one week prior to the initiation of the
10.1520/E2784–10.
test.Activityofthetestmaterialismeasuredbycomparingthe
Federal Register, Vol 46, No. 17, Jan 27, 1991.
For referenced ASTM standards, visit the ASTM website, www.astm.org, or
contact ASTM Customer Service at service@astm.org. For Annual Book of ASTM
Standards volume information, refer to the standard’s Document Summary page on Technical Manual of the American Association of Textile Chemists and
the ASTM website. Colorists, P.O. Box 12215, Research Triangle Park, North Carolina 27709.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959. United States
E2784 − 10
number of test organisms recovered from artificially contami- 6.5.1 Water Faucet(s)—To be located above the sink at a
nated hands after use of a handwashing formulation to the height which permits the hands to be held higher than the
numberrecoveredfromcontaminatedhandsnotexposedtothe elbowduringthewashingprocedure.Faucetshouldmaintaina
test formulation. The method describes specific procedures to flow rate of 4 L per minute, as determined in (10.3).
be followed using Serratia marcescens as the test organism. 6.5.2 Tap Water Temperature Regulator and Temperature
The activity of the test material is measured following a single Monitor—To monitor and regulate water temperature of
wash in a single day using a neutralization recovery method. 40 62°C.
4.2 Alternative test organisms which may be used are 6.6 Vortex Mixer—Any suitable vortex mixer capable of
Escherichia coli, Shigella flexneri,and Staphylococcus aureus. mixing sample and diluent.
Culture media and incubation conditions appropriate for the
6.7 Sterile Bacteriological Pipets—1.1, 2.2, 5.0, and 30.0
alternative organisms should be employed.
mL capacity.
4.3 The investigator should be aware that there may be
6.8 Adjustable or Fixed Volume Pipets and Sterile Tips—0.1
health risks associated with the use of the test organisms and
mL and 1.0 mL capacity.
precautions similar to those referenced in 8.5 should be
6.9 Sampling Containers—Any sterile or sterilizable con-
undertaken.
tainer having tight closures and sufficient capacity to hold 75
mL sampling solution (7.3).
5. Significance and Use
6.10 Sterile Container—Any sterile or sterilizable container
5.1 Thisprocedurehasbeendesignedtoevaluatehandwash
havingthecapacitytoculturetheamountofinoculumrequired
products using a palmar surface only contamination method.
for testing.
This method is an alternative contamination procedure to that
listed in Test Method E1174. The current contamination 6.11 Gloves—Loose-fitting, unlined, powder-free gloves
procedure in Test Method E1174 describes a standardized
which possess no antimicrobial properties, or equivalent.
procedure for contaminating the entire hand, palmar surface Performazoneofinhibitiontest,suchasAATCCTestMethod
andback,directlyusingamarkerorganism.Thecontamination
147, to evaluate the antibacterial activity. (Plastic bags (6.12)
procedureinTestMethodE1174doesnotnecessarilyrepresent with low bioburden may be used in place of gloves.)
real world hand contamination. During routine activities it is
6.12 Plastic Bags—May be used in place of gloves (6.11).
only the palmar surface, comprising palms, fingers, and finger
Bags should be approximately 29 by 31 cm, possess no
pads of the hands that becomes contaminated by contact with
antimicrobial properties, and have a low bioburden. Perform a
transient microorganisms. These microorganisms can then be
zone of inhibition test, such as AATCC Test Method 147, to
transferred to food or objects. Methods to measure the amount
evaluate the antibacterial activity.
of microorganisms transferred to food or objects can be found
5 6
6.13 Wrist Ties or Tourniquets—Any item which will allow
in Fischler et al and Fuls et al and will be developed into a
the plastic bags (6.12) or gloves (6.11) to be secured to the
future ASTM standard.
subject’s wrist.
6. Apparatus 6.14 Sterile Paper Towel Pouches—Each pouch consists of
two single-ply paper towels, each of which measures approxi-
6.1 Colony Counter—Anyofseveraltypesmaybeused,for
mately 20 by 32 6 5 cm, encased in aluminum foil.
example, Quebec Colony Counter.
6.14.1 Fold two single-ply paper towels in half, lengthwise
6.2 Incubator—Any incubator capable of maintaining the
to form a rectangle approximately 20 by 16 cm. Place one
following temperatures: S. marcescens (25 6 2°C—this tem-
paper towel inside of the other.
perature is required to ensure pigment production for S.
6.14.2 Place the paper towels in a piece of aluminum foil
marcescens); S. aureus, E. coli, S. flexneri (35 6 2°C).
which has been folded in half, widthwise. The aluminum foil
6.3 Sterilizer—Any suitable steam sterilizer capable of pro- should measure approximately 38 by 23 cm, after folding.
ducing the conditions of sterilization is acceptable. Aluminum foil which is rated as “Heavy Duty” and has a
minimum thickness of 0.2 mm is recommended to minimize
6.4 Timer (Stop-Clock)—One that can be read for minutes
the risk of tearing during handling. Fold the edges of the
and seconds.
aluminumfoiltogethertoformapouchensuringthatthepaper
6.5 Handwashing Sink—A sink of sufficient size to permit
towels remain flat. Sterilize the pouch by autoclaving.
subjects to wash without touching hands to sink surface or
6.15 Sterile Centrifuge Tubes—Minimum of 50 mL capac-
other subjects.
ity.
7. Reagents and Materials
Fischler, et al, “Effect of Hand Wash Agents on Controlling the Transmission
7.1 Cleansing Wash—A mild, proven, non-antimicrobial
of Pathogenic Bacteria from Hands to Food,” Journal of Food Protection, Vol 70,
No. 12, 2007, pp. 2873–2877.
soft soap. The formula in Table 1 can be used if a mild,
Fuls, et al, “Alternative Hand Contamination Techniques to Compare the
non-antimicrobial soft soap is not commercially available.
Activities of Antimicrobial and Nonantimicrobial Soaps Under Different Test
7.1.1 Add linseed oil to a solution of potassium hydroxide
Conditions,” Applied and Environmental Microbiology ,Vol 74, No. 12, June 2008,
pp. 3739–3744. in 15 parts water and heat up to approximately 70°C while
E2784 − 10
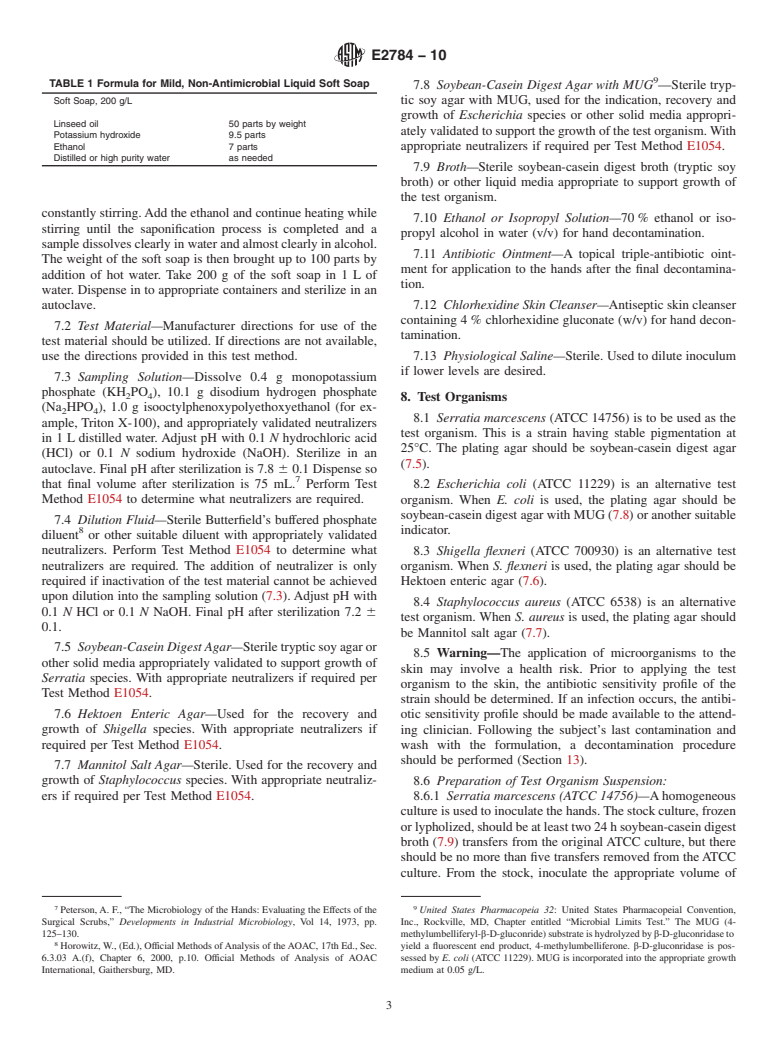
TABLE 1 Formula for Mild, Non-Antimicrobial Liquid Soft Soap
7.8 Soybean-Casein Digest Agar with MUG —Sterile tryp-
Soft Soap, 200 g/L tic soy agar with MUG, used for the indication, recovery and
growth of Escherichia species or other solid media appropri-
Linseed oil 50 parts by weight
atelyvalidatedtosupportthegrowthofthetestorganism.With
Potassium hydroxide 9.5 parts
Ethanol 7 parts appropriate neutralizers if required per Test Method E1054.
Distilled or high purity water as needed
7.9 Broth—Sterile soybean-casein digest broth (tryptic soy
broth) or other liquid media appropriate to support growth of
the test organism.
constantlystirring.Addtheethanolandcontinueheatingwhile
7.10 Ethanol or Isopropyl Solution—70% ethanol or iso-
stirring until the saponification process is completed and a
propyl alcohol in water (v/v) for hand decontamination.
sampledissolvesclearlyinwaterandalmostclearlyinalcohol.
7.11 Antibiotic Ointment—A topical triple-antibiotic oint-
The weight of the soft soap is then brought up to 100 parts by
ment for application to the hands after the final decontamina-
addition of hot water. Take 200 g of the soft soap in 1 L of
tion.
water. Dispense in to appropriate containers and sterilize in an
7.12 Chlorhexidine Skin Cleanser—Antisepticskincleanser
autoclave.
containing 4% chlorhexidine gluconate (w/v) for hand decon-
7.2 Test Material—Manufacturer directions for use of the
tamination.
test material should be utilized. If directions are not available,
use the directions provided in this test method. 7.13 Physiological Saline—Sterile. Used to dilute inoculum
if lower levels are desired.
7.3 Sampling Solution—Dissolve 0.4 g monopotassium
phosphate (KH PO ), 10.1 g disodium hydrogen phosphate
2 4
8. Test Organisms
(Na HPO ), 1.0 g isooctylphenoxypolyethoxyethanol (for ex-
2 4
8.1 Serratia marcescens (ATCC 14756) is to be used as the
ample, Triton X-100), and appropriately validated neutralizers
test organism. This is a strain having stable pigmentation at
in 1 L distilled water.Adjust pH with 0.1 N hydrochloric acid
25°C. The plating agar should be soybean-casein digest agar
(HCl) or 0.1 N sodium hydroxide (NaOH). Sterilize in an
(7.5).
autoclave. Final pH after sterilization is 7.8 6 0.1 Dispense so
that final volume after sterilization is 75 mL. Perform Test 8.2 Escherichia coli (ATCC 11229) is an alternative test
Method E1054 to determine what neutralizers are required.
organism. When E. coli is used, the plating agar should be
soybean-caseindigestagarwithMUG(7.8)oranothersuitable
7.4 Dilution Fluid—Sterile Butterfield’s buffered phosphate
indicator.
diluent or other suitable diluent with appropriately validated
neutralizers. Perform Test Method E1054 to determine what 8.3 Shigella flexneri (ATCC 700930) is an alternative test
neutralizers are required. The addition of neutralizer is only
organism. When S. flexneri is used, the plating agar should be
required if inactivation of the test material cannot be achieved Hektoen enteric agar (7.6).
upon dilution into the sampling solution (7.3).Adjust pH with
8.4 Staphylococcus aureus (ATCC 6538) is an alternative
0.1 N HCl or 0.1 N NaOH. Final pH after sterilization 7.2 6
test organism. When S. aureus is used, the plating agar should
0.1.
be Mannitol salt agar (7.7).
7.5 Soybean-CaseinDigestAgar—Steriletrypticsoyagaror
8.5 Warning—The application of microorganisms to the
other solid media appropriately validated to support growth of
skin may involve a health risk. Prior to applying the test
Serratia species. With appropriate neutralizers if required per
organism to the skin, the antibiotic sensitivity profile of the
Test Method E1054.
strain should be determined. If an infection occurs, the antibi-
7.6 Hektoen Enteric Agar—Used for the recovery and otic sensitivity profile should be made available to the attend-
growth of Shigella species. With appropriate neutralizers if ing clinician. Following the subject’s last contamination and
required per Test Method E1054.
wash with the formulation, a decontamination procedure
should be performed (Section 13).
7.7 Mannitol Salt Agar—Sterile. Used for the recovery and
growth of Staphylococcus species. With appropriate neutraliz-
8.6 Preparation of Test Organism Suspension:
ers if required per Test Method E1054. 8.6.1 Serratia marcescens (ATCC 14756)—Ahomogeneous
cultureisusedtoinoculatethehands.Thestockculture,frozen
orlypholized,shouldbeatleasttwo24hsoybean-caseindigest
broth (7.9) transfers from the originalATCC culture, but there
should be no more than five transfers removed from theATCC
culture. From the stock, inoculate the appropriate volume of
7 9
Peterson,A. F., “The Microbiology of the Hands: Evaluating the Effects of the United States Pharmacopeia 32: United States Pharmacopeial Convention,
Surgical Scrubs,” Developments in Industrial Microbiology, Vol 14, 1973, pp. Inc., Rockville, MD, Chapter entitled “Microbial Limits Test.” The MUG (4-
125–130. methylumbelliferyl-β-D-gluconride)substrateishydrolyzedbyβ-D-gluconridaseto
Horowitz,W., (Ed.), Off
...






Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.