ASTM E2799-11
(Test Method)Standard Test Method for Testing Disinfectant Efficacy against Pseudomonas aeruginosa Biofilm using the MBEC Assay
Standard Test Method for Testing Disinfectant Efficacy against <span class="italic">Pseudomonas aeruginosa</span> Biofilm using the MBEC Assay
SIGNIFICANCE AND USE
Vegetative biofilm bacteria are phenotypically different from suspended planktonic cells of the same genotype. Biofilm growth reactors are engineered to produce biofilms with specific characteristics. Altering either the engineered system or operating conditions will modify those characteristics. The goal in biofilm research and efficacy testing is to choose the growth reactor that generates the most relevant biofilm for the particular study.
The purpose of this test method is to direct a user in how to grow, treat, sample and analyze a Pseudomonas aeruginosa biofilm using the MBEC Assay. Microscopically, the biofilm is sheet-like with few architectural details as seen in Harrison et al (5). The MBEC Assay was originally designed as a rapid and reproducible assay for evaluating biofilm susceptibility to antibiotics (2). The engineering design allows for the simultaneous evaluation of multiple test conditions, making it an efficient method for screening multiple disinfectants or multiple concentrations of the same disinfectant. Additional efficiency is added by including the neutralizer controls within the assay device. The small well volume is advantageous for testing expensive disinfectants, or when only small volumes of the disinfectant are available.
SCOPE
1.1 This test method specifies the operational parameters required to grow and treat a Pseudomonas aeruginosa biofilm in a high throughput screening assay known as the MBEC (trademarked) (Minimum Biofilm Eradication Concentration) Physiology and Genetics Assay. The assay device consists of a plastic lid with ninety-six (96) pegs and a corresponding receiver plate with ninety-six (96) individual wells that have a maximum 200 μL working volume. Biofilm is established on the pegs under batch conditions (that is, no flow of nutrients into or out of an individual well) with gentle mixing. The established biofilm is transferred to a new receiver plate for disinfectant efficacy testing. The reactor design allows for the simultaneous testing of multiple disinfectants or one disinfectant with multiple concentrations, and replicate samples, making the assay an efficient screening tool.
1.2 This test method defines the specific operational parameters necessary for growing a Pseudomonas aeruginosa biofilm, although the device is versatile and has been used for growing, evaluating and/or studying biofilms of different species as seen in Refs (1-4).
1.3 Validation of disinfectant neutralization is included as part of the assay.
1.4 This test method describes how to sample the biofilm and quantify viable cells. Biofilm population density is recorded as log colony forming units per surface area. Efficacy is reported as the log reduction of viable cells.
1.5 Basic microbiology training is required to perform this assay.
1.6 The values stated in SI units are to be regarded as standard. No other units of measurement are included in this standard.
1.7 ASTM International takes no position respecting the validity of any patent rights asserted in connection with any item mentioned in this standard. Users of this standard are expressly advised that determination of the validity of any such patent rights, and the risk of infringement of such rights, are entirely their own responsibility.
1.8 This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety and health practices and determine the applicability of regulatory limitations prior to use.
General Information
Relations
Standards Content (Sample)
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Please contact ASTM International (www.astm.org) for the latest information.
Designation: E2799 – 11
Standard Test Method for
Testing Disinfectant Efficacy against Pseudomonas
aeruginosa Biofilm using the MBEC Assay
This standard is issued under the fixed designation E2799; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (´) indicates an editorial change since the last revision or reapproval.
1. Scope 1.5 Basic microbiology training is required to perform this
assay.
1.1 This test method specifies the operational parameters
1.6 The values stated in SI units are to be regarded as
required to grow and treat a Pseudomonas aeruginosa biofilm
standard. No other units of measurement are included in this
in a high throughput screening assay known as the MBEC
standard.
(trademarked) (Minimum Biofilm Eradication Concentration)
1.7 ASTM International takes no position respecting the
Physiology and GeneticsAssay. The assay device consists of a
validity of any patent rights asserted in connection with any
plastic lid with ninety-six (96) pegs and a corresponding
item mentioned in this standard. Users of this standard are
receiver plate with ninety-six (96) individual wells that have a
expressly advised that determination of the validity of any such
maximum 200 µL working volume. Biofilm is established on
patent rights, and the risk of infringement of such rights, are
the pegs under batch conditions (that is, no flow of nutrients
entirely their own responsibility.
into or out of an individual well) with gentle mixing. The
1.8 This standard does not purport to address all of the
established biofilm is transferred to a new receiver plate for
,
3 4
safety concerns, if any, associated with its use. It is the
disinfectant efficacy testing. The reactor design allows for
responsibility of the user of this standard to establish appro-
the simultaneous testing of multiple disinfectants or one
priate safety and health practices and determine the applica-
disinfectant with multiple concentrations, and replicate
bility of regulatory limitations prior to use.
samples, making the assay an efficient screening tool.
1.2 This test method defines the specific operational param-
2. Referenced Documents
eters necessary for growing a Pseudomonas aeruginosa bio-
2.1 ASTM Standards:
film, although the device is versatile and has been used for
E1054 Test Methods for Evaluation of Inactivators of An-
growing, evaluating and/or studying biofilms of different
5 timicrobial Agents
species as seen in Refs (1-4).
2.2 Other Standards:
1.3 Validation of disinfectant neutralization is included as
Method 9050 Buffered Dilution Water Preparation accord-
part of the assay.
ing to Eaton et al (5)
1.4 This test method describes how to sample the biofilm
and quantify viable cells. Biofilm population density is re-
3. Terminology
corded as log colony forming units per surface area. Efficacy is
3.1 Definitions:
reported as the log reduction of viable cells.
3.1.1 biofilm, n—microorganisms living in a self-organized,
cooperativecommunityattachedtosurfaces,interfaces,oreach
This test method is under the jurisdiction of ASTM Committee E35 on
other, embedded in a matrix of extracellular polymeric sub-
Pesticides, Antimicrobials, and Alternative Control Methods and is the direct
stances of microbial origin, while exhibiting an altered pheno-
responsibility of Subcommittee E35.15 on Antimicrobial Agents.
type with respect to growth rate and gene transcription.
Current edition approved April 1, 2011. Published April 2011. DOI: 10.1520/
E2799–11. 3.1.1.1 Discussion—Biofilms may be comprised of bacte-
The MBEC trademark is held by Innovotech, Inc., Edmonton,Alberta, Canada.
ria, fungi, algae, protozoa, viruses, or infinite combinations of
The sole source of supply of the apparatus known to the committee at this time
these microorganisms. The qualitative characteristics of a
is Innovotech Inc., Edmonton, Alberta, Canada. If you are aware of alternative
biofilm including, but not limited to, population density,
suppliers, please provide this information to ASTM International Headquarters.
Your comments will receive careful consideration at a meeting of the responsible
taxonomic diversity, thickness, chemical gradients, chemical
technical committee, which you may attend.
TheMBECAssayiscoveredbyapatent.Interestedpartiesareinvitedtosubmit
information regarding the identification of an alternative(s) to this patented item to
the ASTM International Headquarters. Your comments will receive careful consid- For referenced ASTM standards, visit the ASTM website, www.astm.org, or
eration at a meeting of the responsible technical committee, which you may attend. contact ASTM Customer Service at service@astm.org. For Annual Book of ASTM
The boldface numbers in parentheses refer to a list of references at the end of Standards volume information, refer to the standard’s Document Summary page on
this standard. the ASTM website.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959, United States.
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Please contact ASTM International (www.astm.org) for the latest information.
E2799 – 11
composition,consistency,andothermaterialsinthematrixthat reproducible assay for evaluating biofilm susceptibility to
arenotproducedbythebiofilmmicroorganisms,arecontrolled antibiotics (2). The engineering design allows for the simulta-
by the physicochemical environment in which it exists. neous evaluation of multiple test conditions, making it an
3.1.2 disinfectant, n—chemicals used on inanimate surfaces efficient method for screening multiple disinfectants or mul-
to rapidly inactivate 99.9 % of the treated microorganisms at a tiple concentrations of the same disinfectant. Additional effi-
specific concentration and desired exposure time. ciency is added by including the neutralizer controls within the
3.2 Definitions of Terms Specific to This Standard: assay device. The small well volume is advantageous for
3.2.1 peg, n—biofilm sample surface (base: 5.0 mm, height: testing expensive disinfectants, or when only small volumes of
13.1 mm). the disinfectant are available.
3.2.2 peg lid, n—an86 3128mmplasticsurfaceconsisting
6. Apparatus
of ninety-six (96) identical pegs.
3.2.3 plate, n—an 86 3 128 mm standard plate consisting
6.1 Inoculating loop—nichrome wire or disposable plastic.
of ninety-six (96) identical wells.
6.2 Petri dish—square 100 3 100 3 15 mm, plastic, sterile.
3.2.4 well, n—small reservoir with a 50 to 200 µL working
6.3 Microcentrifuge tubes—sterile, any with a 1.5 mL
volume capacity.
volume capacity.
3.3 Acronyms:
6.4 96-wellmicrotiterplate—sterile,86 3128mmstandard
3.3.1 ATCC—American Type Culture Collection
plate consisting of ninety-six (96) identical flat bottom wells
3.3.2 BGC—biofilm growth check
with a 200 µL working volume.
3.3.3 CFU—colony forming unit
NOTE 1—Alignment corner must be in the H12 position of the plate for
3.3.4 MBEC—minimum biofilm eradication concentration
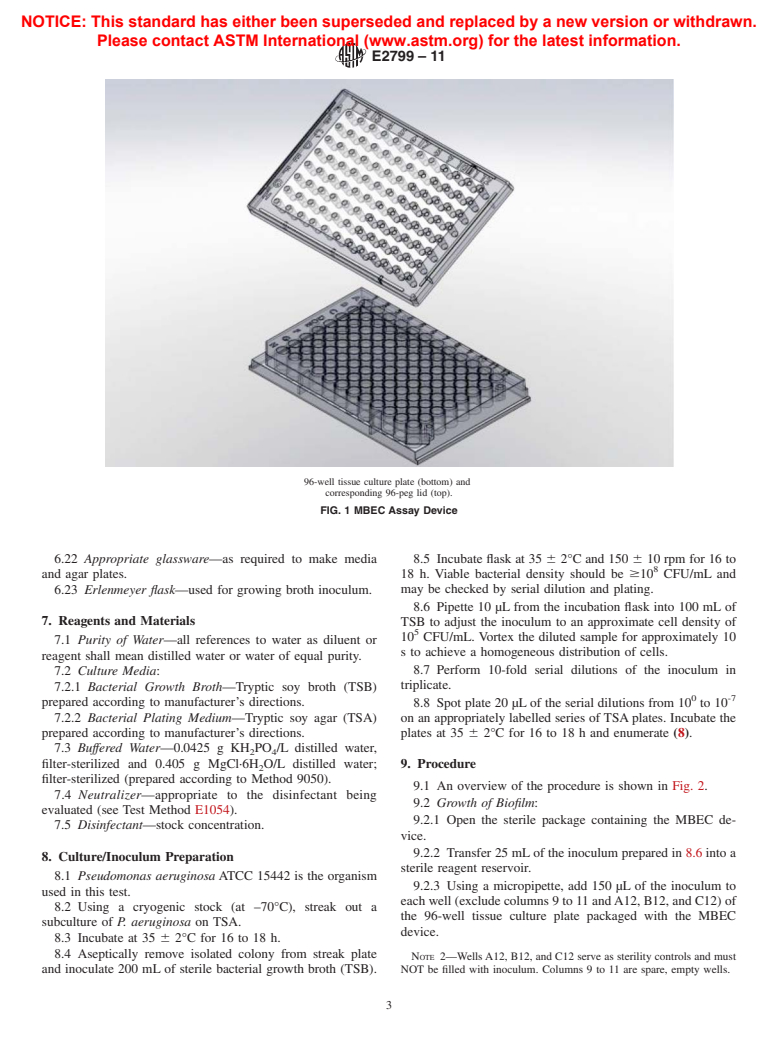
proper alignment with the MBEC lid (see Fig. 1).
3.3.5 rpm—revolutions per minute
6.5 Vortex—any vortex that will ensure proper agitation and
3.3.6 SC—sterility control
mixing of microfuge tubes.
3.3.7 TSA—tryptic soy agar
6.6 Bath sonicator—any capable of an average sonic power
3.3.8 TSB—tryptic soy broth
of 180 W in a dry environment (7).
3.3.9 UC—untreated control
6.7 Stainless steel insert tray—for bath sonicator.
4. Summary of Test Method
6.8 Bunsen burner—used to flame-sterilize inoculating loop
(if metal) and other instruments.
4.1 This test method describes the use of the MBEC Assay
6.9 95 % Ethanol—used to flame-sterilize pliers.
in evaluating the efficacy of a disinfectant against a Pseudomo-
6.10 4-in. bent needle nose pliers—for aseptic removal and
nas aeruginosa biofilm. A mature biofilm is established on
handling of pegs.
pegs under batch conditions with very low shear produced by
6.11 Pipette—continuously adjustable pipette with volume
gentle rotation of the device on an orbital shaker.At the end of
capability of 1 mL.
24 h of growth, the pegs containing the biofilm are rinsed to
6.12 Micropipette—continuously adjustable pipette with
remove planktonic cells and the peg lid is placed in a receiver
working volume of 10 to 200 µL.
plate. The wells in the receiver plate are filled according to an
6.13 Sterile pipette tips—200 µL and 1000 µL volumes.
experimental design that contains the appropriate sterility,
6.14 Sterile reagent reservoir—50 mL polystyrene.
growth, and neutralizer controls as well as the disinfectants.
6.15 Analytical balance—sensitive to 0.01 g.
Afteraspecifiedcontacttime,thepeglidisplacedinareceiver
6.16 Sterilizer—any steam sterilizer capable of producing
plate containing neutralizer, and the entire device is placed in
the conditions of sterilization.
a sonicator to remove the biofilm and disaggregate the clumps.
6.17 Colony counter—any one of several types may be
Samples from each well are then diluted, plated and the viable
used. A hand tally for the recording of the bacterial count is
cellsenumerated.Thelogreductioninviablecellsiscalculated
recommended if manual counting is done.
bysubtractingthemeanlogdensityforthetreatedbiofilmfrom
6.18 Environmental incubator—capable of maintaining a
the mean log density determined for the untreated controls.
temperatureof35 62°Candrelativehumiditybetween35and
5. Significance and Use
85 %.
5.1 Vegetative biofilm bacteria are phenotypically different 6.19 Orbitalshaker—capableofmaintaininganorbitof110
to 150 rpm.
from suspended planktonic cells of the same genotype. Biofilm
growth reactors are engineered to produce biofilms with 6.20 Reactor components—the MBEC Assay device is
shown in Fig. 1. Fig. 3 is a diagram of the challenge plate.
specific characteristics. Altering either the engineered system
6.21 Sterile conical tubes—50 mL, used to prepare initial
or operating conditions will modify those characteristics. The
inoculum.
goal in biofilm research and efficacy testing is to choose the
growth reactor that generates the most relevant biofilm for the
particular study.
5.2 Thepurposeofthistestmethodistodirectauserinhow
The sole source of microtiter plates (Nunclon (trademarked) Catalogue No.
167008) that provide reproducible results is Thermo Fisher Scientific, Waltham,
to grow, treat, sample and analyze a Pseudomonas aeruginosa
MA, USA, www.thermofisher.com. If you are aware of alternative suppliers, please
biofilm using the MBECAssay. Microscopically, the biofilm is
provide this information toASTM International Headquarters. Your comments will
sheet-like with few architectural details as seen in Harrison et 1
receive careful consideration at a meeting of the responsible technical committee,
al(5).TheMBECAssaywasoriginallydesignedasarapidand which you may attend.
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Please contact ASTM International (www.astm.org) for the latest information.
E2799 – 11
96-well tissue culture plate (bottom) and
corresponding 96-peg lid (top).
FIG. 1 MBEC Assay Device
6.22 Appropriate glassware—as required to make media 8.5 Incubate flask at 35 6 2°C and 150 6 10 rpm for 16 to
and agar plates. 18 h. Viable bacterial density should be$10 CFU/mL and
6.23 Erlenmeyer flask—used for growing broth inoculum. may be checked by serial dilution and plating.
8.6 Pipette 10 µL from the incubation flask into 100 mL of
7. Reagents and Materials TSB to adjust the inoculum to an approximate cell density of
10 CFU/mL. Vortex the diluted sample for approximately 10
7.1 Purity of Water—all references to water as diluent or
s to achieve a homogeneous distribution of cells.
reagent shall mean distilled water or water of equal purity.
8.7 Perform 10-fold serial dilutions of the inoculum in
7.2 Culture Media:
triplicate.
7.2.1 Bacterial Growth Broth—Tryptic soy broth (TSB)
0 -7
prepared according to manufacturer’s directions. 8.8 Spot plate 20 µL of the serial dilutions from 10 to 10
7.2.2 Bacterial Plating Medium—Tryptic soy agar (TSA) on an appropriately labelled series of TSAplates. Incubate the
prepared according to manufacturer’s directions. plates at 35 6 2°C for 16 to 18 h and enumerate (8).
7.3 Buffered Water—0.0425 g KH PO /L distilled water,
2 4
filter-sterilized and 0.405 g MgCl·6H O/L distilled water; 9. Procedure
filter-sterilized (prepared according to Method 9050).
9.1 An overview of the procedure is shown in Fig. 2.
7.4 Neutralizer—appropriate to the disinfectant being
9.2 Growth of Biofilm:
evaluated (see Test Method E1054).
9.2.1 Open the sterile package containing the MBEC de-
7.5 Disinfectant—stock concentration.
vice.
9.2.2 Transfer 25 mLof the inoculum prepared in 8.6 into a
8. Culture/Inoculum Preparation
sterile reagent reservoir.
8.1 Pseudomonas aeruginosa ATCC 15442 is the organism
9.2.3 Using a micropipette, add 150 µL of the inoculum to
used in this test.
each well (exclude columns 9 to 11 andA12, B12, and C12) of
8.2 Using a cryogenic stock (at –70°C), streak out a
the 96-well tissue culture plate packaged with the MBEC
subculture of P. aeruginosa on TSA.
device.
8.3 Incubate at 35 6 2°C for 16 to 18 h.
8.4 Aseptically remove isolated colony from streak plate
NOTE 2—WellsA12, B12, and C12 serve as sterility controls and must
and inoculate 200 mL of sterile bacterial growth broth (TSB). NOT be filled with inoculum. Columns 9 to 11 are spare, empty wells.
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Please contact ASTM International (www.astm.org) for the latest information.
E2799 – 11
FIG. 2 A Flow Diagram Representing the MBEC Assay for Disinfectant Testing
9.2.4 Place the peg lid onto the microtiter plate. Ensure that 9.4.3 Add 200 µL of sterile TSB to well A12 of the
the orientation of the plate matches the orientation of the lid challenge plate. This will serve as the device sterility control
(that is, pegA1 must be inserted into wellA1 of the microtiter (SC).
plate, otherwise the device will not fit together correctly, see
9.4.4 Add 200 µLof sterile neutralizer to column 7 and well
Fig. 1). Label the device appropriately.
B12. These serve as the neutralizer toxicity control (N) and
sterility control.
NOTE 3—Volumeofinoculumusedinthisstephasbeencalibratedsuch
9.4.5 Add 100 µL of sterile neutralizer to column 6, fol-
that the biofilm covers a surface area that is entirely immersed by the
volume of antimicrobial used in the challenge plate setup (Section 9.4). low
...







Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.