ASTM F1608-00
(Test Method)Standard Test Method for Microbial Ranking of Porous Packaging Materials (Exposure Chamber Method)
Standard Test Method for Microbial Ranking of Porous Packaging Materials (Exposure Chamber Method)
SCOPE
1.1 This test method is used to determine the passage of airborne bacteria through porous materials intended for use in packaging sterile medical devices. This test method is designed to test materials under conditions that result in the detectable passage of bacterial spores through the test material.
1.1.1 A round-robin study was conducted with eleven laboratories participating. Each laboratory tested duplicate samples of six commercially available porous materials to determine the LRV. Materials tested under the standard conditions described in this test method returned average values that range from LRV 1.7 to 4.3.
1.1.2 Results of this round-robin study indicate that caution should be used when comparing test data and ranking materials, especially when a small number of sample replicates are used. In addition, further collaborative work (such as described in Practice E691) should be conducted before this test method would be condsidered adequate for purposes of setting performance standards.
1.2 This test method requires manipulation of microorganisms and should be performed only by trained personnel. The U.S. Department of Health and Human Services publication Biosafety in Microbiological and Biomedical Laboratories (CDC/NIH-HHS Publication No. 84-8395) should be consulted for guidance.
1.3 This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety and health practices and determine the applicability of regulatory limitations prior to use.
General Information
Relations
Standards Content (Sample)
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Contact ASTM International (www.astm.org) for the latest information
Designation: F 1608 – 00
Standard Test Method for
Microbial Ranking of Porous Packaging Materials (Exposure
Chamber Method)
This standard is issued under the fixed designation F 1608; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (e) indicates an editorial change since the last revision or reapproval.
1. Scope E 691 Practice for Conducting an Interlaboratory Study to
Determine the Precision of a Test Method
1.1 This test method is used to determine the passage of
airborne bacteria through porous materials intended for use in
3. Terminology
packaging sterile medical devices. This test method is designed
3.1 Definition:
to test materials under conditions that result in the detectable
3.1.1 porous packaging material, n—a material used in
passage of bacterial spores through the test material.
medical packaging which is intended to provide an environ-
1.1.1 A round-robin study was conducted with eleven labo-
mental and biological barrier, while allowing sufficient air flow
ratories participating. Each laboratory tested duplicate samples
to be used in gaseous sterilization methods (for example, EO,
of six commercially available porous materials to determine
steam, gas plasma).
the LRV. Materials tested under the standard conditions de-
scribed in this test method returned average values that range
4. Summary of Test Method
from LRV 1.7 to 4.3.
4.1 Samples of porous materials are subjected to an aerosol
1.1.2 Results of this round-robin study indicate that caution
of Bacillus subtilis var. niger spores within an exposure
should be used when comparing test data and ranking materi-
chamber. Spores which pass through the porous sample are
als, especially when a small number of sample replicates are
collected on membrane filters and enumerated. The logarithm
used. In addition, further collaborative work (such as described
reduction value (LRV) is calculated by comparing the loga-
in Practice E 691) should be conducted before this test method
rithm of the number of spores passing through the porous
would be condsidered adequate for purposes of setting perfor-
material with the logarithm of the microbial challenge.
mance standards.
4.2 Standard Set of Conditions—This test method specifies
1.2 This test method requires manipulation of microorgan-
a standard set of conditions for conducting the exposure
isms and should be performed only by trained personnel. The
chamber test method. A standard set of conditions is required to
U.S. Department of Health and Human Services publication
enable evaluation of materials between laboratories. The con-
Biosafety in Microbiological and Biomedical Laboratories
ditions stated in this test method were chosen for several
(CDC/NIH-HHS Publication No. 84-8395) should be con-
reasons. First, it is difficult to maintain an aerosol of spores
sulted for guidance.
over long periods of time. (Also, if the spore challenge time is
1.3 This standard does not purport to address all of the
long, the cost of the test increases). Second, to determine the
safety concerns, if any, associated with its use. It is the
differences between materials, it is necessary to test the
responsibility of the user of this standard to establish appro-
materials under conditions which allow passage of bacterial
priate safety and health practices and determine the applica-
spores. If a material does not allow any passage of spores, all
bility of regulatory limitations prior to use.
that can be stated is that it has better resistance to penetration
2. Referenced Documents than the severity of the challenge conditions. Third, it is
necessary to have a large spore challenge level to be able to
2.1 ASTM Standards:
detect the passage of spores through the entire range of
E 177 Practice for Use of the Terms Precision and Bias in
2 commercially available porous packaging materials. The stan-
ASTM Test Methods
dard conditions stated in this test method are based upon these
factors. (Additional information may be found in the Refer-
This test method is under the jurisdiction of ASTM Committee F-2 on Flexible ences section). However, since many factors influence the
Barrier Materials and is the direct responsibility of Subcommittee F02.60 on
determination of an appropriate porous material (outlined in
Medical Packaging.
5.1.1-5.1.4), each user may modify these conditions (that is,
Current edition approved April 10, 2000. Published June 2000. Originally
bacterial challenge, time, flow rate) after first conducting
published as F 1608–95. Last previous edition F 1608–95.
Annual Book of ASTM Standards, Vol 14.02.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959, United States.
F1608–00
studies at the specified standard conditions. The standard set of can be influenced by factors including the free-air volume
target parameters for conducting the test method are as follows: within the package and pressure changes occurring as a result
4.2.1 Flow Rate Through Sample—2.8 L/min.
of transportation, manipulation, weather, or mechanical influ-
4.2.2 Exposure Time— 15 min.
ences (such as room door closures and HVAC systems).
4.2.3 Target Microbial Challenge—1 3 10 colony forming
5.1.4 The microstructure of a porous material which influ-
units (CFU)/sample port.
ences the relative ability to adsorb or entrap microorganisms,
or both, under different air-flow conditions.
5. Significance and Use
5.1 The exposure-chamber method is a quantitative proce-
6. Apparatus
dure for determining the microbial-barrier properties of porous
materials under the conditions specified by the test. Data 6.1 This procedure should be conducted in a microbiologi-
obtained from this test are useful in assessing the relative
cal laboratory by trained personnel. As a result, it is assumed
potential of a particular porous material to contribute to the loss
that basic microbiological equipment and supplies for conduct-
of sterility to the contents of the package versus another porous
ing routine microbiological manipulations (that is, standard
material. This test method is not intended to predict the
plate counts, sterilization with an autoclave, and so forth) will
performance of a given material in a specific sterile-packaging
be available.
application. The maintenance of sterility in a particular pack-
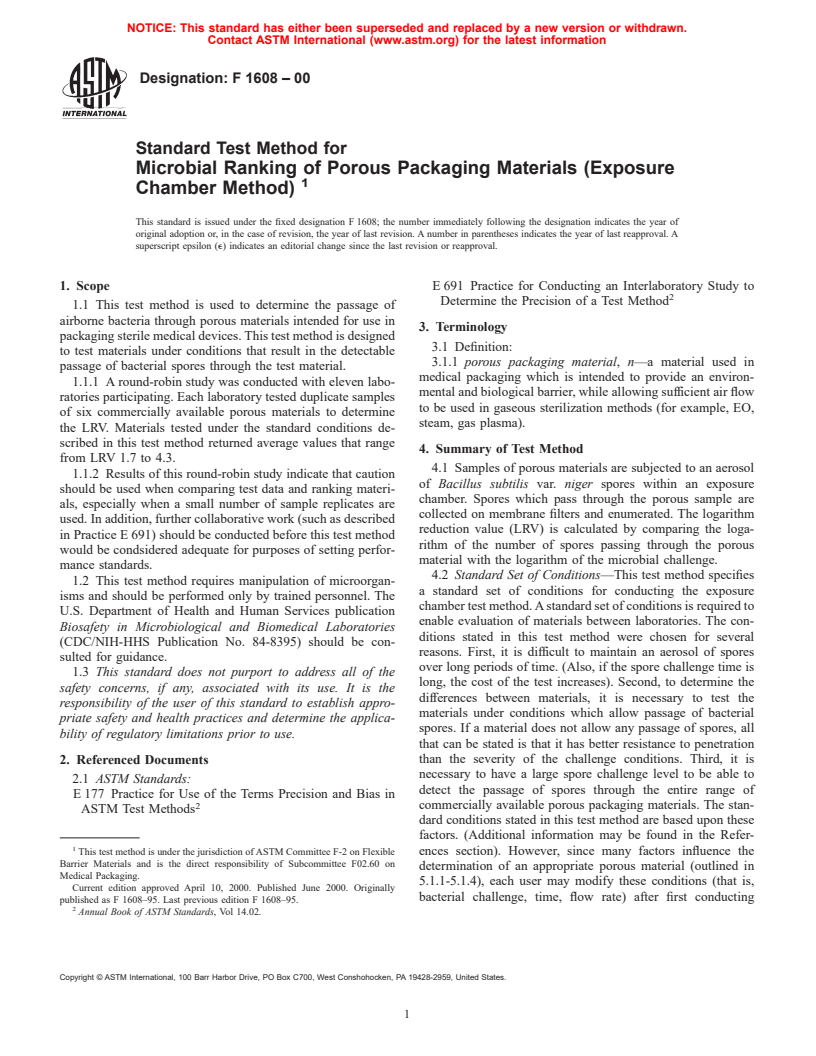
6.2 Exposure Chamber, constructed primarily from acrylic
aging application will depend on a number of factors, includ-
sheeting and consists of two major sections, as illustrated in
ing, but not limited to the following:
Fig. 1. The bottom section contains a six-place manifold
5.1.1 The bacterial challenge (number and kinds of micro-
connected to six flowmeters, one per port, containing hoses
organisms) that the package will encounter in its distribution
attached to six filtering units. The port to the manifold is
and use. This may be influenced by factors such as shipping
attached to a vacuum source. A vacuum gage is mounted
methods, expected shelf life, geographic location, and storage
between the manifold and the vacuum source. The upper
conditions.
chamber contains a fan for dispersion of the bacterial aerosol,
5.1.2 The package design, including factors such as adhe-
a port for attachment of the nebulizer, a port for exhausting the
sion between materials, the presence or absence of secondary
chamber, and a plate for attachment of disposable or steriliz-
and tertiary packaging, and the nature of the device within the
able filter units. The chamber may use disposable filter units or
package.
5.1.3 The rate and volume exchange of air that the porous reusable filter units, or both.
package encounters during its distribution and shelf life. This
FIG. 1 Exposure Chamber
F1608–00
7. Materials 9. Apparatus Preparation
7.1 Bacillus subtilis var. niger (ATCC9372), aqueous spore
9.1 Since aerosols containing bacterial spores are formed
suspension in water.
during the use of this apparatus, the exposure chamber (see Fig.
7.2 Soybean Casein Digest Agar—Bottles for pour plates
1) should be assembled and used within a biological safety
and pre-poured plates (;25 mL in 100 by 15-mm plates)
cabinet.
prepared commercially or in accordance with standard tech-
9.1.1 Place the top of the chamber on the bottom base.
niques.
9.1.2 Connect the top of each of the six flowmeters to the
7.3 Sterile Cellulose Nitrate Filters, 47 or 50-mm diameter,
manifold using 0.65-cm inside diameter hoses. Connect the
depending upon filter unit specification, 0.45-μm pore size.
manifold to a filtered vacuum source.
7.4 Sterile Bottle-Top Filter Units, (Falcon-type 7104 or
9.1.3 Connect the bottom of each sample flowmeter to a
filter holders with funnel 310-4000 or equivalent).
filter unit with 0.65-cm inside diameter hose using an end
7.5 Glass Nebulizer.
connector.
7.6 Sterile Forceps.
9.1.4 Using a rubber hose, attach the nebulizer to a tee
7.7 Incubator, 30 to 35°C.
connector made of a 0.65-cm PVC and three pieces of 0.6-cm
7.8 Disk Cutter, 47 or 50-mm diameter, depending upon
inside diameter PVC piping approximately 7.5 cm long.
filter unit specification.
9.1.5 Attach the vertical leg of the tee to a trap jar using a
7.9 Sterile Gloves.
rubber stopper with a 0.65-cm diameter hole. The trap jar is
7.10 Sterile Syringe, 3-cm with needle or micropipette.
intended to retain any unsuspended droplets produced by the
7.11 Sterile Pipettes, to deliver 0.1, 1, 10, and 25 mL.
nebulizer.
7.12 Blender, with sterile ⁄2-pt jar(s).
9.1.6 Attach the second end of the tee to a 1.3-cm inside
7.13 Vortex Mixer.
diameter rubber tubing approximately 3.8 cm long and connect
7.14 Vacuum Pump, with air filter.
to the front port of the chamber.
7.15 Calibrated Timer.
9.1.7 Attach a 1.3-cm inside diameter rubber tubing ap-
7.16 Calibrated Flowmeters—One each with a range from 5
proximately 16 cm long to the mouth of the nebulizer. Connect
to 30 L/min; six each with a range from 1.0 to 5.0 L/min.
the loose end of the tubing to the third end of the tee.
7.17 Sterile Petri Plates.
9.1.8 Connect the nebulizer inlet port with a 0.5-cm inside
7.18 Sterile Water, 100 and 9.9-mL aliquots, or other
diameter rubber tubing to the top port of a calibrated flowmeter
appropriate volumes for membrane grinding and dilutions.
(from 5 to 30-L/min range).
7.19 Hoses and Piping— See Section 9 for lengths and
9.1.9 Connect the bottom port of the nebulizer to a filtered
diameters.
air source.
7.20 Rubber Stoppers with Holes—See Section 9 for sizes.
9.1.10 Attach the exhaust port of the chamber that is used
7.21 Trap Jar.
for evacuation to a 1.3-cm inside diameter tubing which, in
7.22 Calibrated Vacuum Gage.
turn, leads to an air filter and to a vacuum source.
7.23 Compressed Air Source, with air filter.
9.2 Filter Unit-Holder Preparation:
7.24 Biocontainment Hood.
9.2.1 Wrap each non-sterile sterilizable filter unit in a
7.25 Chlorine Bleach, or suitable sporocide.
sterilizable wrap.
8. Sample Preparation
9.2.2 Sterilize the filter units as specified by the manufac-
turer. Presterilized filter units do not need to be resterilized.
8.1 Cut random samples of material into disks in accordance
with the size required for the filter holder being used (47 or 50
10. Apparatus Validation
mm) using a disk cutter. It is suggested that additional samples
be cut to allow for errors during the procedure. Typically, the
10.1 The test apparatus (see Fig. 1) must be validated for
sample disks are sterilized prior to testing using a test method
bacterial challenge to each port. This step should be performed
appropriate for the specific material. Materials may also be
upon first use of the chamber and a minimum of three runs
tested before or after they are subjected to other conditions
should be conducted. The following description outlines vali-
such as heat or cold, relative humidity, different sterilization
dation of the test procedure for a challenge of 1 3 10 colony
processes, real time, or accelerated aging. The samples may be
forming units (CFU) per port in 15 min at a flow rate of 2.8
stored in sterile petri plates or other suitable sterile containers
L/min. If testing is to be conducted using other parameters, a
before testing.
validation should be conducted using those parameters.
8.2 The minimum sample size for a given material is two,
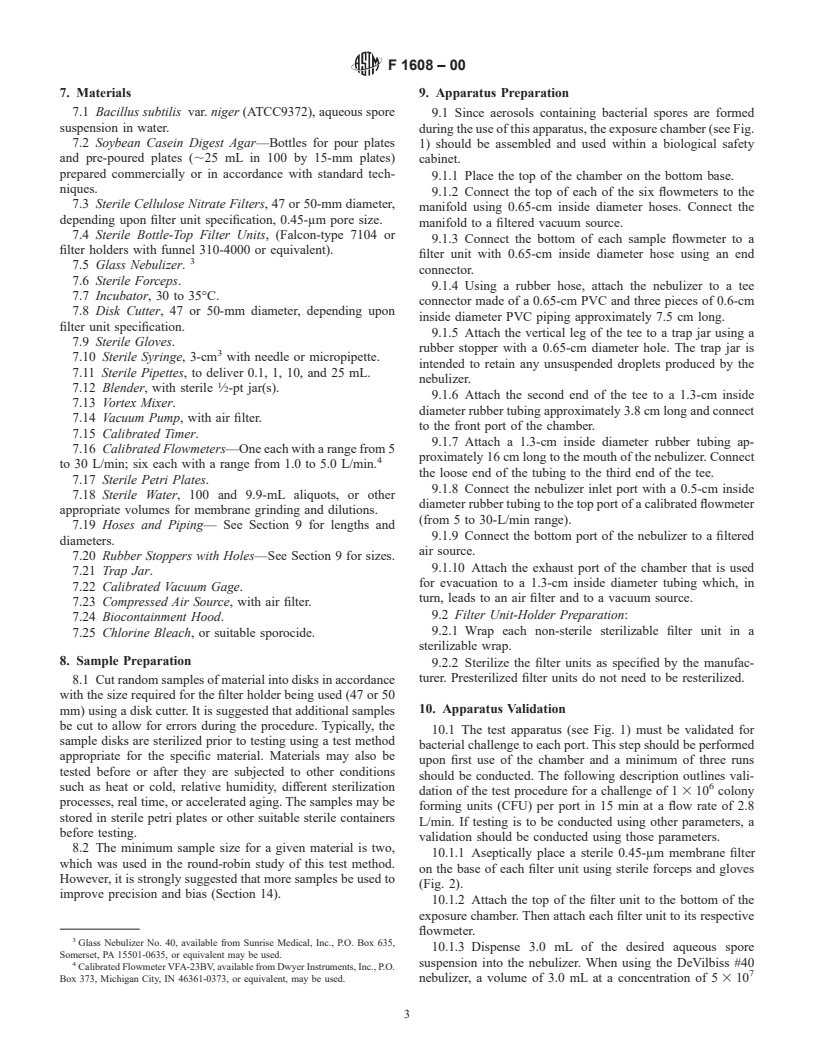
10.1.1 Aseptically place a sterile 0.45-μm membrane filter
which was used in the round-robin study of this test method.
on the base of each filter unit using sterile forceps and gloves
However, it is strongly suggested that more samples be used to
(Fig. 2).
improve precision and bias (Section 14).
10.1.2 Attach the top of the filter unit to the bottom of the
exposure chamber. Then attach each filter unit to its respective
flowmeter.
Glass Nebulizer No. 40, available from Sunrise Medical, Inc., P.O. Box 635,
10.1.3 Dispense 3.0 mL of the desired aqueous spore
Somerset, PA 15501-0635, or equivalent may be used.
suspension into the nebulizer. When using the DeVilbiss #40
Calibrated Flowmeter VFA-23BV, available from Dwyer Instruments, Inc., P.O.
Box 373, Michigan City, IN 46361-0373, or equivalent, may be used. nebulizer, a volume of 3.0 mL at a concentration of 5 3 10
F1608–00
10.1.11 Disconnect the hoses from each of the filter units,
and remove the units from the bottom plate of the chamber.
10.1.12 Remove the filter membranes aseptically, one at a
time, and enumerate the organisms on each membrane (Fig. 3).
Since more than 100 CFU are anticipated, the spores must be
eluted from the membrane by grinding the membrane for 1 min
in a ⁄2-pt sterile blender jar containing 100.0 mL of sterile
water. Samples are then serially diluted prior to performing
standard plate counts to accurately determine the number of
spores. A dilution and plating scheme, which was used in the
round-robin study, includes plating 10.0, 1.0, and 0.1-mL
aliquots of the blended membrane in duplicate. An additional 1
to 100 dilution is prepared by placing 0.1 mL in 9.9 mL of
sterile water and plating 1.0 and 0.1-mL aliquots of this
dilution in duplicate. This scheme produces dilution factors of
−1 −2 −3 −4 −5
10 ,10 ,10 ,10 , and 10 . Other dilution protocols may
be used. Plates having between 25 and 250 CFU should be
used for enumeration. If alternative test conditions are used,
then the previously described dilution scheme may not be
appropriate. In instances where colony counts are less than 30
CFU, the limit of detection is dependent upon the volume of
the undiluted aliquot plated from the blender jar. Duplicate
10-m
...






Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.