ASTM F2148-07(2012)
(Practice)Standard Practice for Evaluation of Delayed Contact Hypersensitivity Using the Murine Local Lymph Node Assay (LLNA)
Standard Practice for Evaluation of Delayed Contact Hypersensitivity Using the Murine Local Lymph Node Assay (LLNA)
SIGNIFICANCE AND USE
5.1 The propensity of a material to stimulate delayed contact hypersensitivity must be assessed before clinical application of devices containing this material. Delayed hypersensitivity may occur anywhere in the body. Systemic delayed hypersensitivity may have a complex set of reactions and consequences depending on the actual tissue/organ site of reaction. Although the reactions are seldom life-threatening, severe tissue and organ damage my result over time. Skin is the usual test site to determine the propensity of a material to cause delayed hypersensitivity.
5.2 The standard historical test methods have involved the use of guinea pigs with a cutaneous application and observation of the reaction site. The use of the murine local lymph node assay results in a numerical quantitation of stimulation, rather than subjective evaluation and could be used to determine dose responses.
5.3 This practice may not be predictive of events occurring during all types of implant applications. The user is cautioned to consider the appropriateness of the method in view of the materials being tested, their potential applications, and the recommendations contained in Practice F748.
SCOPE
1.1 This practice provides a methodology to use an in-situ procedure for the evaluation of delayed contact hypersensitivity reactions.
1.2 This practice is intended to provide an alternative to the use of guinea pigs for evaluation of the ability of a device material to stimulate delayed contact hypersensitivity reactions. This alternative is particularly applicable for materials used in devices that contact only intact skin. However, the guinea pig maximization test is still the recommended method when assessing the delayed hypersensitivity response to metals or when testing substances that do not penetrate the skin but are used in devices that contact deep tissues or breached surfaces. The guinea pig maximization test should be used for these substances.
1.3 This practice consists of a protocol for assessing an increase in lymphocyte proliferation within the nodes draining the site of administration on the ears of mice.
1.4 The LLNA has been validated only for low-molecular-weight chemicals that can penetrate the skin. The absorbed chemical or metabolite must bind to macromolecules, such as proteins, to form immunogenic conjugates.
1.5 This practice is one of several developed for the assessment of the biocompatibility of materials. Practice F748 may provide guidance for the selection of appropriate methods for testing materials for a specific application.
1.6 Identification of a supplier of materials or reagents is for the convenience of the user and does not imply a single source. Appropriate materials and reagents may be obtained from many commercial supply houses.
1.7 The values stated in SI units are to be regarded as standard. No other units of measurement are included in this standard.
1.8 This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety and health practices and determine the applicability of regulatory limitations prior to use.
General Information
Relations
Standards Content (Sample)
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Contact ASTM International (www.astm.org) for the latest information
Designation: F2148 − 07(Reapproved 2012)
Standard Practice for
Evaluation of Delayed Contact Hypersensitivity Using the
Murine Local Lymph Node Assay (LLNA)
This standard is issued under the fixed designation F2148; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (´) indicates an editorial change since the last revision or reapproval.
1. Scope 1.8 This standard does not purport to address all of the
safety concerns, if any, associated with its use. It is the
1.1 This practice provides a methodology to use an in-situ
responsibility of the user of this standard to establish appro-
procedure for the evaluation of delayed contact hypersensitiv-
priate safety and health practices and determine the applica-
ity reactions.
bility of regulatory limitations prior to use.
1.2 This practice is intended to provide an alternative to the
2. Referenced Documents
use of guinea pigs for evaluation of the ability of a device
material to stimulate delayed contact hypersensitivity reac- 2
2.1 ASTM Standards:
tions. This alternative is particularly applicable for materials
F619 Practice for Extraction of Medical Plastics
used in devices that contact only intact skin. However, the
F720 PracticeforTestingGuineaPigsforContactAllergens:
guinea pig maximization test is still the recommended method
Guinea Pig Maximization Test
when assessing the delayed hypersensitivity response to metals
F748 PracticeforSelectingGenericBiologicalTestMethods
orwhentestingsubstancesthatdonotpenetratetheskinbutare
for Materials and Devices
used in devices that contact deep tissues or breached surfaces.
F750 Practice for Evaluating Material Extracts by Systemic
The guinea pig maximization test should be used for these
Injection in the Mouse
substances.
2.2 Other Document:
ICCVAM NIH Publication No: 99-4494 The Murine Local
1.3 This practice consists of a protocol for assessing an
increase in lymphocyte proliferation within the nodes draining Lymph Node Assay, 1999
the site of administration on the ears of mice.
3. Terminology
1.4 The LLNA has been validated only for low-molecular-
3.1 Definitions:
weight chemicals that can penetrate the skin. The absorbed
3.1.1 AOO, n—acetone olive oil solution (4:1 v/v) is a
chemical or metabolite must bind to macromolecules, such as
suitable nonpolar solvent.
proteins, to form immunogenic conjugates.
3.1.2 aqueous solvent, n—in this assay refers to the polar
1.5 This practice is one of several developed for the
solvent, saline.
assessment of the biocompatibility of materials. Practice F748
3.1.3 DMSO, n—dimethylsulfoxide (nonaqueous, suitable
may provide guidance for the selection of appropriate methods
organic solvent).
for testing materials for a specific application.
3.1.4 DNCB, n—2,4-dinitrochlorobenzene.
1.6 Identification of a supplier of materials or reagents is for
3.1.5 formalin, n—a ⁄10 dilution of 37 to 39 % formalde-
the convenience of the user and does not imply a single source.
hyde solution (formaldehyde) in PBS.
Appropriate materials and reagents may be obtained from
many commercial supply houses.
3.1.6 ICCVAM, n—Interagency Coordinating Committee on
the Validation of Alternative Methods.
1.7 The values stated in SI units are to be regarded as
standard. No other units of measurement are included in this 3.1.7 nonaqueous solvent, n—in this assay refers to the
standard.
organic or nonpolar solvent, which shall be dimethylsulfoxide
(DMSO) or acetone olive oil (AOO).
1 2
ThispracticeisunderthejurisdictionofASTMCommitteeF04onMedicaland For referenced ASTM standards, visit the ASTM website, www.astm.org, or
Surgical Materials and Devices and is the direct responsibility of Subcommittee contact ASTM Customer Service at service@astm.org. For Annual Book of ASTM
F04.16 on Biocompatibility Test Methods. Standards volume information, refer to the standard’s Document Summary page on
Current edition approved Oct. 1, 2012. Published October 2012. Originally the ASTM website.
ε1 3
approved in 2001. Last previous edition approved in 2007 as F2148 – 07 . DOI: Available from NICEATM, NIEHS, 79 Alexander Dr., Mail Drop EC-17,
10.1520/F2148-07R12. Research Triangle Park, NC 27709.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959. United States
F2148 − 07 (2012)
3.1.8 PBS, n—phosphate buffered saline, pH 7.2. hydroxyethyl cellulose to each 10 mL of the aqueous vehicle
control and test solutions to aid in holding the solution to the
3.1.9 positive control, n—a substance capable of consis-
ear.
tently stimulating lymphocyte proliferation.
6.4 The final specimen to be extracted should be prepared
3.1.10 saline, n—0.9 % sodium chloride (aqueous, polar
with a surface finish consistent with end-use application.
solvent).
6.5 The specimen shall be sterilized by the method to be
3.1.11 TCA, n—5 % trichloroacetic acid.
H3 used for the final product.
3.1.12 tritiated thymidine, n— methyl thymidine, specific
activity 2 Ci/mM (in PBS) I IUDR-radioactive uridine. 6.6 Care should be taken that the specimens do not become
contaminated during preparation and aseptic technique is
3.1.13 vehicle controls, n—an aqueous, polar solvent and a
recommended.
non-aqueous, nonpolar solvent.
7. Preparation of Positive Controls
4. Summary of Practice
7.1 Nonaqueous Positive Control—Weigh0.025gofDNCB
4.1 Test and control substances or extracts are applied to the
and place in a flask. Add enough DMSO to dissolve all of the
ears of test mice. The draining lymph nodes are harvested and
DNCB.Add more DMSO to bring the level up to 10 mL. Cap
lymphocyte proliferation evaluated. Comparisons are made
and shake the flask until a homogeneous solution is obtained.
with the control and test specimens tested under identical
The dose level of the positive control should not produce
conditions.
systemic toxicity as evidenced by clinical observations.
7.2 Aqueous Positive Control—Neutral buffered formalin is
5. Significance and Use
commercially available. (Or dilute formaldehyde ⁄10 in PBS.
5.1 The propensity of a material to stimulate delayed
Place 1 mL of formaldehyde in a 10-mL flask. Add enough
contact hypersensitivity must be assessed before clinical ap-
PBS to mix the two solutions.Add more PBS to bring the level
plication of devices containing this material. Delayed hyper-
up to 10 mL. Cap and shake the flask until a homogeneous
sensitivity may occur anywhere in the body. Systemic delayed
solution is obtained.)
hypersensitivity may have a complex set of reactions and
7.3 Aqueous solutions are not suitable for application to the
consequences depending on the actual tissue/organ site of
ear. Therefore, for use in the assay, add 0.05 g of hydroxyethyl
reaction. Although the reactions are seldom life-threatening,
cellulose to each 10 mLof the aqueous positive control to aid
severetissueandorgandamagemyresultovertime.Skinisthe
in holding the solution to the ear until absorbed.
usualtestsitetodeterminethepropensityofamaterialtocause
delayed hypersensitivity.
7.4 For all specimens requiring extractions, prepare an
aqueous and non-aqueous extract (DMSO or AOO are recom-
5.2 The standard historical test methods have involved the
mended but other permissible extractants are listed in the
use of guinea pigs with a cutaneous application and observa-
ICCVAM document) following the procedures described in
tion of the reaction site. The use of the murine local lymph
Practice F619.
node assay results in a numerical quantitation of stimulation,
rather than subjective evaluation and could be used to deter-
8. Dosing of the Animals
mine dose responses.
8.1 Healthy, non-pregnant female CBA/Ca or CBA/j mice
5.3 This practice may not be predictive of events occurring
that are seven to twelve weeks of age shall be used. House the
during all types of implant applications. The user is cautioned
animals according to treatment group with five animals per
to consider the appropriateness of the method in view of the
cage.
materials being tested, their potential applications, and the
8.2 Day One—Uniquelyidentifyeachmouse(eartagsorear
recommendations contained in Practice F748.
notches may not be used). Weigh each mouse to the nearest
whole gram.
6. Preparation of Test Specimens
8.3 Aminimum of five mice shall be used for each positive
6.1 Specimens should be prepared in accordance with Prac-
andnegativecontrolandeachtestsample.Theyshallbetreated
tice F619. All solid materials shall be extracted. Extractions
dailyforthreeconsecutivedaysbytopicalapplicationof25µL
shall be done with an aqueous (polar) solvent and a nonaque-
of one of the solutions to the dorsal surface of both ears. For
ous (nonpolar or organic) solvent, either DMSO or AOO.
the aqueous groups only, the dorsal surface should be wiped
6.2 Liquid test articles and gels shall be used directly if they
with acetone just before treating to aid in absorption of the
are not irritants.Aliquid that is an irritant shall be diluted with
aqueous solution, although it will not be completely absorbed.
an aqueous or nonaqueous solvent based on solubility of the
liquid test article until the solution is non-irritating.
“Final Report on the Safety Assessment of Hydroxyethylcellulose,
6.3 Wholly aqueous solutions are not suitable for applica-
Hydroxypropylcellulose, Methylcellulose, Hydroxypropyl Methylcellulose, and
tion to the ear. Therefore, for use in the assay, add 0.05 g of Cellulose Gum,” J. Amer Coll Tox., Vol 5, No. 3, 1986, pp. 1-59.
F2148 − 07 (2012)
8.3.1 For testing, other than liquid test articles, the groups cpm
5 dpm
shall include: aqueous and nonaqueous positive controls, decimal counter efficiency
aqueous and nonaqueous vehicle controls, aqueous extract of
For verification of the working tritiated thymidine solution,
the test sample, and nonaqueous extract of test sample.
determinetheclosenessoftheconcentrationto80µCi/mL.The
8.3.2 For testing of liquid test articles, the groups shall
final diluted solution contains 0.032 µCi. Since 1.0
include: aqueous and nonaqueous positive controls, the liquid
µCi = 2 220 000 dpm, then 0.032 µCi = 71 040 dpm. There-
test sample, and either an aqueous or a nonaqueous vehicle
fore:
control appropriate for the nature of the liquid sample.
mean dpm
8.3.3 The extract shall be used within 24 h of preparation.
the µCi of the working solution 5 380 µCi/mL
71040 dpm
The extract should be stored in a stoppered container at room
temperature. The applications shall be performed at 24 62h
Make adjustments to the solution as needed. Make similar
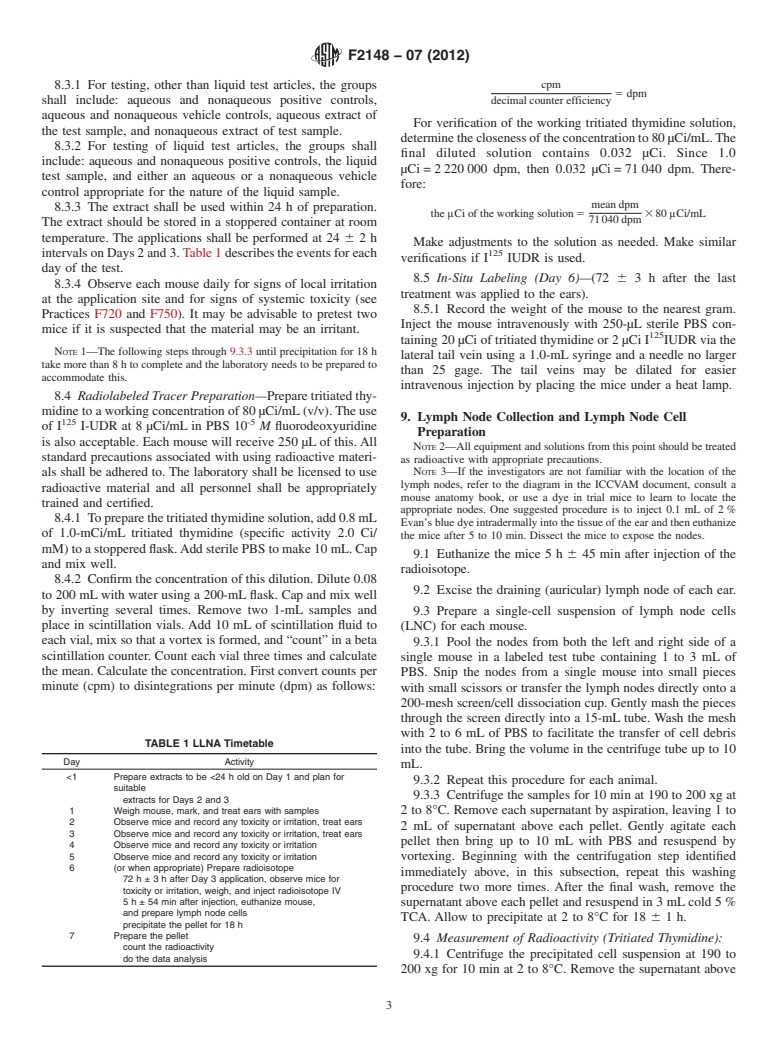
intervalsonDays2and3.Table1describestheeventsforeach
verifications if I IUDR is used.
day of the test.
8.5 In-Situ Labeling (Day 6)—(72 6 3 h after the last
8.3.4 Observe each mouse daily for signs of local irritation
treatment was applied to the ears).
at the application site and
...






Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.