ASTM F2151-01
(Practice)Standard Practice for Assessment of White Blood Cell Morphology After Contact with Materials (Withdrawn 2007)
Standard Practice for Assessment of White Blood Cell Morphology After Contact with Materials (Withdrawn 2007)
SCOPE
1.1 This practice provides a protocol for the assessment of the effect of materials used in the fabrication of medical devices, that will contact blood, on the morphology of white blood cells.
1.2 This practice is intended to evaluate the acute in vitro effects of materials intended for use in contact with blood.
1.3 This practice uses direct contact of the material with blood, and extracts of the material are not used.
1.4 This practice is one of several developed for the assessment of the biocompatibility of materials. Practice F 748 provides general guidance for the selection of appropriate methods for testing materials for a specific application.
1.5 This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety and health practices and determine the applicability of regulatory limitations prior to use.
1.6 Identification of a supplier of materials or reagents is for the convenience of the user and does not imply single source. Appropriate materials and reagents may be obtained from many commercial supply houses.
WITHDRAWN RATIONALE
This practice provides a protocol for the assessment of the effect of materials used in the fabrication of medical devices, that will contact blood, on the morphology of white blood cells.
Formerly under the jurisdiction of Committee F04 on Medical and Surgical Materials and Devices, this practice was withdrawn in February 2007 because it is no longer valid.
General Information
Standards Content (Sample)
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Contact ASTM International (www.astm.org) for the latest information
Designation: F 2151 – 01
Standard Practice for
Assessment of White Blood Cell Morphology After Contact
with Materials
This standard is issued under the fixed designation F 2151; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (e) indicates an editorial change since the last revision or reapproval.
1. Scope 3.1.1 control material, n—a material such as low density
polyethylene (LDPE) which is expected to have minimal effect
1.1 This practice provides a protocol for the assessment of
on the morphology of white blood cells.
the effect of materials used in the fabrication of medical
3.1.2 nuclear damage, n—for the white blood cell morphol-
devices, that will contact blood, on the morphology of white
ogy test, this term us used to describe the nucleus of a white
blood cells.
blood cell appears to be condensed, fragmented or lysed; for
1.2 This practice is intended to evaluate the acute in vitro
the White Blood Cell Morphology Test. This includes nuclear
effects of materials intended for use in contact with blood.
damage that might be classified as karyolysis, karyorrhexis,
1.3 This practice uses direct contact of the material with
pyknosis, or simply necrosis.
blood, and extracts of the material are not used.
3.1.3 positive control material, n—a material such as latex
1.4 This practice is one of several developed for the
(gloves, dental dam, or tubing) or TSV, tin-stabilized vinyl
assessment of the biocompatibility of materials. Practice F 748
(slab), which is expected to have an adverse effect on the
provides general guidance for the selection of appropriate
morphology of white blood cells.
methods for testing materials for a specific application.
3.2 Abbreviations:
1.5 This standard does not purport to address all of the
3.2.1 B—basophil
safety concerns, if any, associated with its use. It is the
3.2.2 BR—broken or lysed
responsibility of the user of this standard to establish appro-
3.2.3 E—eosinophil
priate safety and health practices and determine the applica-
3.2.4 INDNM—indistinct nuclear membrane: a degenera-
bility of regulatory limitations prior to use.
tive change of the nucleus; for the White Blood Cell Morphol-
1.6 Identification of a supplier of materials or reagents is
ogyTest, this term is used to describe a nuclear membrane that
for the convenience of the user and does not imply single
is rough, ragged, or torn
source. Appropriate materials and reagents may be obtained
3.2.5 L—lymphocyte
from many commercial supply houses.
3.2.6 M—monocyte
2. Referenced Documents
3.2.7 N—neutrophil
3.2.8 UNID—unidentified
2.1 ASTM Standards:
F 619 Practice For Extraction Of Medical Plastics
4. Summary of Practice
F 748 Practice For Selecting Generic Biological Test Meth-
2 4.1 Test and control material specimens are exposed to
ods For Materials And Devices
contact with canine blood under defined static conditions and
F 756 Practice for Assessment of Hemolytic Properties of
2 the effect on blood cell morphology is determined. The use of
Materials
human blood is permissible if the laboratory is knowledgeable
3. Terminology of precautions needed to handle human blood. If a source of
blood other than canine or human is used, consideration should
3.1 Definitions:
be given to the differences in hematologic values and morphol-
ogy differences between that species and humans.
5. Significance and Use
ThispracticeisunderthejurisdictionofASTMCommitteeF04onMedicaland
Surgical Materials and Devices and is the direct responsibility of Subcommittee
5.1 The presence of material in contact with the blood may
F04.16 on Biocompatibility Test Methods.
cause damage to white blood cells resulting in changes in
Current edition approved Oct. 10, 2001. Published March 2002.
Annual Book of ASTM Standards, Vol 13.01. function of these cells or changes in properties of the blood.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959, United States.
F2151–01
5.2 This practice may not be predictive of events occurring to the bottom of the vial. Incubate the sample vials for 120 6
during all types of blood contacting applications. The user is 5minwithoutmixingoragitation.Donotsinkfloatersthatrise
cautioned to consider the appropriateness of the method in from the bottom of the vial during the incubation.
view of the materials being tested, their potential applications, 7.4 At the end of the incubation time, remove the vials one
and the recommendations contained in Practice F 748. The at a time, remove the control or test article, and prepare the
propensity of a material to cause hemolysis should be ad- smears as described in Section 8.
dressed according to Practice F 756.
8. Preparation and Staining of Smears
8.1 Preparation of Time Zero Smears—Prepare two accept-
6. Preparation of Test and Control Specimens
able smears from the anticoagulated blood within 1 h after the
6.1 Specimen samples should be prepared according to
blood was drawn. An automated instrument may be used.
Practice F 619. Direct contact of the material with blood will
8.1.1 An acceptable smear has the following characteristics:
be studied, the blood is the extractant, and other extracts of the
smooth appearance, a feathered edge, and a slight margin on
material are not used. Prepare a sample size such that 1 mL of
both sides of the length of the slide.
blood is used. If the sample size is such that larger volumes of
8.1.2 Quicklydrythesmearsbywavingtheslidesrapidlyin
bloodareneeded,thisispermissiblebutnoteinthereport.This
the air to prevent distortion of the cells. Label the two smears
scale up would be based on an expected sample size of 3
2 with the following: date of preparation, Time 0, A, or B.
cm /mL.
8.1.3 When dry, stain the blood smears using Wright-
6.2 The final sample should be prepared with a surface
Giemsastain(orappropriatestaindesignatedforbloodsmears)
finish consistent with end-use application.
following the instructions. Purified water, which is neutral,
6.3 The sample shall be sterilized by the method to be used
rather than tap water, which may be alkaline, or distilled water,
for the final product.
which may be acidic, should be used to control the pH in the
6.4 Care should be taken that the specimens do not become
rinse stage. Lean the slides in a vertical position to dry,
contaminated during preparation, but aseptic technique is not
draining from thick portion of smear to the thin area. Do not
required.
accelerate drying with heat, forced air, or other means. Do not
coverslip the slides at this time.
7. Preparation of Blood Sample
8.1.4 Evaluate the Staining Quality—Microscopically scan
7.1 Trained personnel are required for the blood draw and
the smear to locate an area with good white cell distribution.
the EDTA collection tubes should be used. If human blood is
Using the highest magnification possible without the use of oil,
used, extra safety precautions may be needed. Fill the neces-
assess the staining quality of individual white blood cells.
sary numbers of EDTAblood collection tubes from the jugular
There should be clear nuclear-cytoplasmic demarcations, dis-
vein or other appropriate vein using an appropriate size needle.
tinct nuclear chromatin patterns, and cytoplasmic color differ-
The blood collection tube should be filled to capacity. Do not
ences.
withdraw more than 5 mL/kg of blood per day and no more
8.1.5 If the staining quality is not acceptable, additional
than 10 mL/kg/week from any one dog.
time zero smears can be made to correct the staining problem.
Once the correct staining procedure is identified, this should be
NOTE 1—EDTAis the anticoagulant of choice for morphology studies.
Other anticoagulants (heparin, sodium citrate) may also be considered.
noted and then used on the control and test smears.
However, it is not known at this time whether results using other
8.2 Preparation of Control and Test Article Smears:
anticoagulants are comparable to results using EDTA.
8.2.1 After each vial has been incubated at 37°C for 120 6
7.2 Gently rock the collection tube back and forth three 5 min, remove the negative control or test article from the vial
times to mix the anticoagulant with the blood. Record the time
withtweezersallowingasmuchbloodaspossibletodrainfrom
the blood was drawn. Testing should be initiated as soon as the article back into the vial.
possible after the blood was drawn and definitely within 1 h.
8.2.2 Visually inspect the removed article for adherence of
Pool the blood samples and mix well immediately before use. blood or blood clots and record the findings.
Adequate mixing (20 complete inversions by hand) to ensure
8.2.3 Immediately after the negative control or test article is
suspension of all cellular components is necessary just before removed and examined, swirl or rock the vial gently several
preparation of testing and time zero blood smear preparation. times to mix the blood and prepare two acceptable blood
Do not refrigerate the blood before testing. smears as described in 8.1.1. Cells may become fragile after
7.3 Transfer 1 mL of the blood into the vial containing the exposure to biomaterials and therefore should be handled
LDPEnegativecontrolandplaceintothe37°C 62waterbath. gently. Appropriately label each pair of smears with the date,
It is recommended that screw-capped borosilicate glass vials controlortestarticle,andSmearAorB.Allbloodsmearsmust
11 by 48 mm with a 4-mL capacity be used. Dispense the be prepared within4hofthe blood draw.
appropriate volume of blood into the other vials containing the 8.2.4 Stainthesmearsaccordingtotheprotocolidentifiedin
positive control and the test articles. This may be staggered to 8.1.5.
allow for processing time so that incubation times may be 8.3 Preparation for Examination (Optional Procedure for
consistent. Place the vials into the 37°C 6 2 water bath Application of Cover Slip):
immediately after dispensing the blood. Ensure that the test 8.3.1 Whenallsmearsaredry,mountacoverslipbyplacing
articles are covered with blood. It may be necessary to use a small drops or a thin line of mounting medium down the center
plastic pipette tip or wooden applicator stick to push the article of the smear and placing the coverslip on top. Keep the slide
F2151–01
flat allowing the medium to spread and cover the slide. with the next adjacent but not overlapping area.Avoid the very
Coverslipping is recommended if slides are to be archived. edge of the smear and avoid thick streaks of cells. All white
8.3.2 Allow the slides to air dry for at least 6 h. Remove
blood cells encountered must be included in the count. Intact
excess background color from the back of each slide by wiping
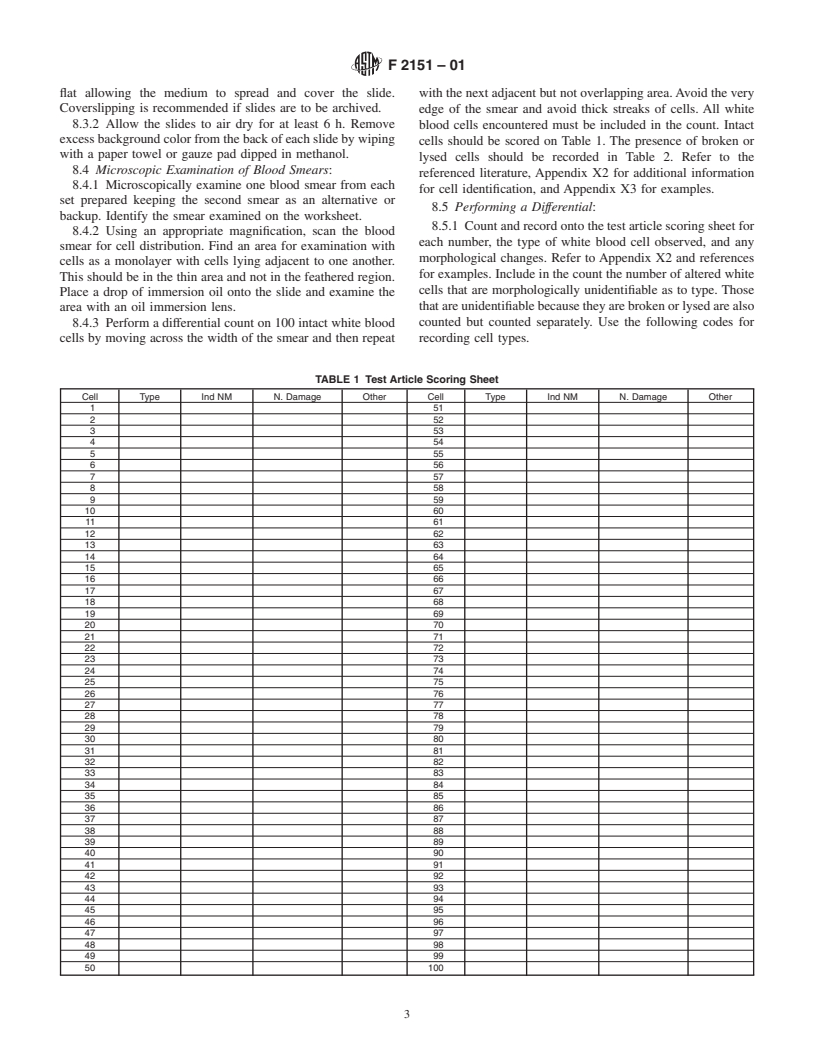
cells should be scored on Table 1. The presence of broken or
with a paper towel or gauze pad dipped in methanol.
lysed cells should be recorded in Table 2. Refer to the
8.4 Microscopic Examination of Blood Smears:
referenced literature, Appendix X2 for additional information
8.4.1 Microscopically examine one blood smear from each
for cell identification, and Appendix X3 for examples.
set prepared keeping the second smear as an alternative or
8.5 Performing a Differential:
backup. Identify the smear examined on the worksheet.
8.5.1 Count and record onto the test article scoring sheet for
8.4.2 Using an appropriate magnification, scan the blood
each number, the type of white blood cell observed, and any
smear for cell distribution. Find an area for examination with
morphological changes. Refer to Appendix X2 and references
cells as a monolayer with cells lying adjacent to one another.
for examples. Include in the count the number of altered white
This should be in the thin area and not in the feathered region.
cells that are morphologically unidentifiable as to type. Those
Place a drop of immersion oil onto the slide and examine the
thatareunidentifiablebecausetheyarebrokenorlysedarealso
area with an oil immersion lens.
8.4.3 Perform a differential count on 100 intact white blood counted but counted separately. Use the following codes for
cells by moving across the width of the smear and then repeat recording cell types.
TABLE 1 Test Article Scoring Sheet
Cell Type Ind NM N. Damage Other Cell Type Ind NM N. Damage Other
1 51
2 52
3 53
4 54
5 55
6 56
7 57
8 58
9 59
10 60
11 61
12 62
13 63
14 64
15 65
16 66
17 67
18 68
19 69
20 70
21 71
22 72
23 73
24 74
25 75
26 76
27 77
28 78
29 79
30 80
31 81
32 82
33 83
34 84
35 85
36 86
37 87
38 88
39 89
40 90
41 91
42 92
43 93
44 94
45 95
46 96
47 97
48 98
49 99
50 100
F2151–01
TABLE 2 Differential
8.6.2 Interpretation:
Cell Expected Range Expected Range % Total 8.6.2.1 If the number of intact white cells, including intact
Identification (Canine) (Human) WBCs
unidentifiable cells, with morphological changes is 4 % or less,
Neutrophil 60–77 % 45–75 %
the test article is considered to not have had an adverse effect
Lymphocyte 12–30 % 16–46 %
Monocyte 3–10 % 4–11 % upon white blood cell morphology (1).
Eosinophil 2–10 % 0–8 %
8.6.2.2 If the number of intact white cells, including intact
Basophil rare <1 % 0–3 %
unidentifiablecells,withmorphologicalchangesisgreaterthan
Unidentified
Number of WBCs scored 100 100
4 %, the test article is considered to have had an adverse effect
Lysed cells
upon white blood cell morphology (1).
8.6.2.3 If the white blood cell differential of the blood in
contact with the material differs from that expected as de-
N = neutrophil,
scribed in 8.6.1, and the number of intact white cells, including
M = monocyte,
intact unidentifiable cells, with morphological changes is 4 %
L = lymphocyte,
E = eosinophil,
or less, count an additional 100 cells to verify.
B = basophil,
8.6.2.4 If the number of intact white cells, including intact
UNID = unidentified, and
unidentifiablecells,withmorphologicalchangesisgreaterthan
BR = broken or lysed.
4 % for the negative control, and/or if the white blood cell
8.5.2 Evaluate the morphological changes while performing
differential of the blood in contact with the negative control
the differential count as “INDNM” for indistinct nuclear
material differs from that expected as described in 8.6.1, count
membrane, “N. damage” for any type of nuclear damage, and
an additional 100 cells to verify. If the results remain the same,
under the column other list the observation such as inclusions,
evaluate the results of the time zero control. If the number of
foamy, etc.
abnormal cells is greater than 4 % for the time zero control,
8.5.3 Aminimumof100cellsmustbecounted.If100intact
then it is rec
...






Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.