ASTM F1629-95(2007)
(Guide)Standard Guide for Establishing Operating Emergency Medical Services and Management Information Systems, or Both (Withdrawn 2015)
Standard Guide for Establishing Operating Emergency Medical Services and Management Information Systems, or Both (Withdrawn 2015)
SCOPE
1.1 The Emergency Medical Services Management Information System (EMS-MIS) serves as a framework for the management and linkage of data documenting the complete emergency episode from onset through the pre-hospital, emergency department, and hospital phases to final discharge. This document establishes a standard guideline for the planning, development, and maintenance of an EMS-MIS framework, including linkage among pre-hospital, hospital, and other public safety or government agencies. The resultant EMS-MIS should be capable of monitoring the compliance of an EMS system with its established system standards, and provide an objective basis upon which different EMS systems can be comparatively evaluated.
1.2 EMS-MIS Goals
1.2.1 To manage data regarding response to a medical emergency.
1.2.2 To provide a process for obtaining and documenting objective, reliable data.
1.2.3 To provide information that can be used to affect operational changes in an EMS system leading to the delivery of better quality emergency medical care.
1.2.4 To provide information to guide the rational investment of local, state, and national resources to improve and maintain EMS.
1.3 This guide will standardize data needed for decision making at various levels of the EMS system, and offer suggestions as to the appropriate use of this information.
1.4 This guide comments on several possible configurations for information flow and data processing, recognizing that no one configuration is best suited to all circumstances.
1.5 This guide focuses on pre-hospital medical activities, including emergency responses, scheduled transports, and all interinstitutional transfers.
1.6 This guide addresses EMS-MIS techniques applicable to the internal operations of outpatient and inpatient facilities as well as pre-hospital care providers.
1.7 This guide will not address specialized data systems and applications such as trauma registries, but will allow for interfacing with such applications.
1.8 This guide will not address computer-aided dispatch (CAD) systems, nor system status management (SSM) applications, but will allow for interfacing with such applications.
WITHDRAWN RATIONALE
This guide established a standard guideline for the planning, development, and maintenance of an EMS-MIS framework.
Formerly under the jurisdiction of Committee F30 on Emergency Medical Services, this guide was withdrawn in June 2015. This guide is being withdrawn without replacement due to its limited use by industry.
General Information
Relations
Standards Content (Sample)
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Contact ASTM International (www.astm.org) for the latest information
Designation: F1629 − 95(Reapproved 2007)
Standard Guide for
Establishing Operating Emergency Medical Services and
Management Information Systems, or Both
This standard is issued under the fixed designation F1629; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (´) indicates an editorial change since the last revision or reapproval.
1. Scope 1.6 ThisguideaddressesEMS-MIStechniquesapplicableto
the internal operations of outpatient and inpatient facilities as
1.1 The Emergency Medical Services Management Infor-
well as pre-hospital care providers.
mation System (EMS-MIS) serves as a framework for the
management and linkage of data documenting the complete
1.7 This guide will not address specialized data systems and
emergency episode from onset through the pre-hospital, emer-
applications such as trauma registries, but will allow for
gency department, and hospital phases to final discharge. This
interfacing with such applications.
document establishes a standard guideline for the planning,
1.8 This guide will not address computer-aided dispatch
development, and maintenance of an EMS-MIS framework,
(CAD) systems, nor system status management (SSM)
including linkage among pre-hospital, hospital, and other
applications, but will allow for interfacing with such applica-
public safety or government agencies. The resultant EMS-MIS
tions.
should be capable of monitoring the compliance of an EMS
system with its established system standards, and provide an
2. Referenced Documents
objective basis upon which different EMS systems can be
comparatively evaluated.
2.1 ASTM Standards:
E622 GuideforDevelopingComputerizedSystems(Discon-
1.2 EMS-MIS Goals:
tinued 2000) (Withdrawn 2000)
1.2.1 To manage data regarding response to a medical
E623 Guide for Developing Functional Requirements for
emergency.
Computerized Systems (Withdrawn 1994)
1.2.2 To provide a process for obtaining and documenting
E624 GuideforDevelopingImplementionDesignsforCom-
objective, reliable data.
puterized Systems (Withdrawn 1994)
1.2.3 To provide information that can be used to affect
operational changes in an EMS system leading to the delivery E625 Guide for Training Users of Computerized Systems
(Discontinued 2000) (Withdrawn 2000)
of better quality emergency medical care.
1.2.4 To provide information to guide the rational invest- E627 Guide for Documenting Computerized Systems (Dis-
continued 2000) (Withdrawn 2000)
ment of local, state, and national resources to improve and
maintain EMS. E730 GuideforDevelopingFunctionalDesignsforComput-
erized Systems (Withdrawn 1994)
1.3 This guide will standardize data needed for decision
E1113 Guide for Project Definition for Computerized Sys-
making at various levels of the EMS system, and offer
tems (Withdrawn 1994)
suggestions as to the appropriate use of this information.
E1239 Practice for Description of Reservation/Registration-
1.4 This guide comments on several possible configurations
Admission, Discharge, Transfer (R-ADT) Systems for
for information flow and data processing, recognizing that no
Electronic Health Record (EHR) Systems
one configuration is best suited to all circumstances.
E1384 Practice for Content and Structure of the Electronic
Health Record (EHR)
1.5 This guide focuses on pre-hospital medical activities,
F1177 Terminology Relating to Emergency Medical Ser-
including emergency responses, scheduled transports, and all
vices
interinstitutional transfers.
1 2
This guide is under the jurisdiction of ASTM Committee F30 on Emergency For referenced ASTM standards, visit the ASTM website, www.astm.org, or
Medical Services and is the direct responsibility of Subcommittee F30.03 on contact ASTM Customer Service at service@astm.org. For Annual Book of ASTM
Organization/Management. Standards volume information, refer to the standard’s Document Summary page on
Current edition approved Feb. 1, 2007. Published February 2007. Originally the ASTM website.
approved in 1995. Last previous edition approved in 2002 as F1629 – 95(2002). The last approved version of this historical standard is referenced on
DOI: 10.1520/F1629-95R07. www.astm.org.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959. United States
F1629 − 95 (2007)
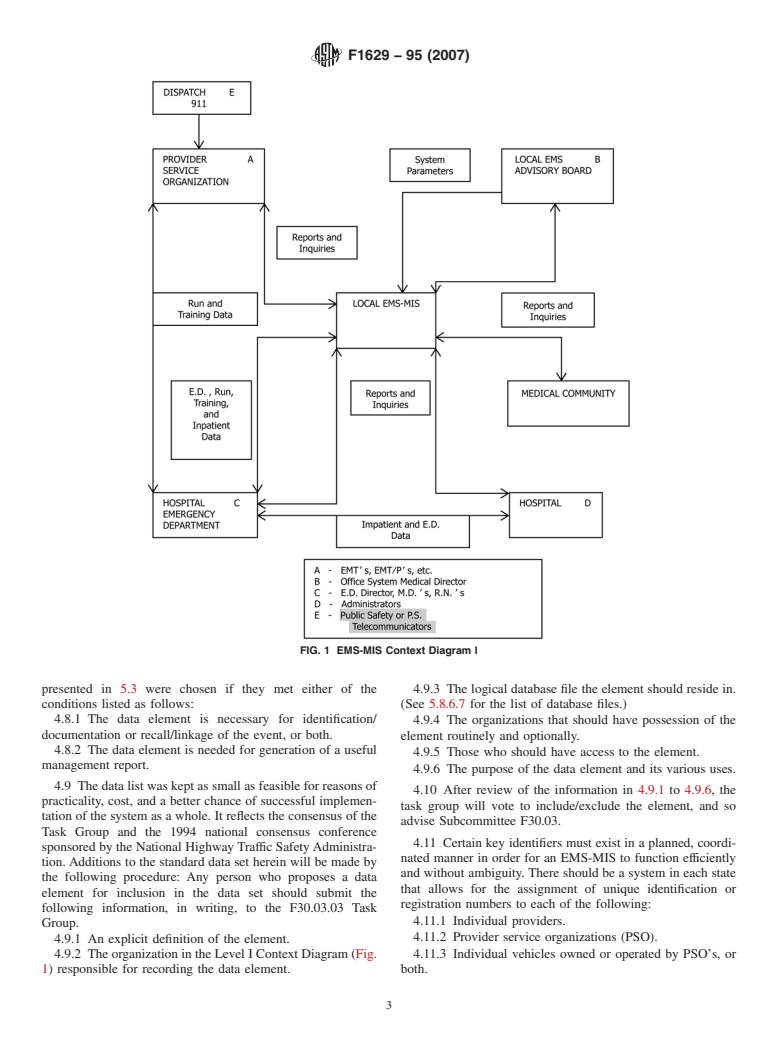
3. Terminology 4.4 Fig. 2 defines the political users of the EMS-MIS. It
should be understood that such entities as LOCAL EMS-MIS,
3.1 Standard EMS terminology is referenced in Terminol-
REMSO, EMS-MIS, and so forth, do not necessarily refer to
ogy F1177. Definition of individual data elements is given in
distinct organizational entities, but may be coordinating divi-
5.3 and 5.4.
sions within the prevailing EMS authority.
3.2 Definitions of Terms Specific to This Standard:
4.5 The EMS-MIS defined herein recognizes a graduated
3.2.1 Continuing Medical Education (CME)—refers to data
process of data collection and analysis. This means that data
that identify all continuing medical education activity com-
elements collected at the provider and hospital levels may be
pleted by an EMT in the system.
useful only at the local levels. Emphasis has been given to the
3.2.2 Data Flow Diagram (DFD)—Diagram that partitions
ability to capture information in an electromagnetic format as
system business functions into a series of events that enhances
closely as possible to the time/source from which it was
analysis and clarifies the purpose, events, and functions that
generated in order to enhance completeness, validity,
take place for each process.
reliability, and utilization of data. By observing the linkage
3.2.3 Emergency Medical Services Management Informa-
parameters defined herein, it should be possible for higher
tionSystem(EMS-MIS)—aframeworkforthemanagementand
levels of the pyramid to access detailed data through wellde-
linkage of data documenting the complete emergency episode
fined linkage mechanisms, when and if necessary, without
from onset through the pre-hospital, emergency department,
resorting to costly duplication and centralization of all data
and hospital phases to final discharge.
elements.
3.2.4 Patient Care Record (PCR)—refers to the data ele-
4.6 The task group recommends that the data collected by
ments described in 5.3 which are to be completed by each PSO
the PSO be aggregated at the various levels that have respon-
for every patient who is treated or transported, or both.
sibility for medical quality assurance, planning, and manage-
3.2.5 Provider Service Organization (PSO)—any public
ment activities. These levels include but are not limited to the
service or commercial organization that utilizes providers to
emergency department, hospital(s), regional EMS, and state-
deliver pre-hospital emergency medical care, and transports
wide.
patients to healthcare facilities, on either an emergency or
4.6.1 The emergency department is an important link be-
prescheduled, non-emergent basis.
tween the pre-hospital and inpatient settings.
3.2.6 Public Safety Answering Point (PSAP)—a dispatch
4.6.2 The medical direction for a PSO, on-line and fre-
center that receives incoming calls for help.
quently off-line as well, usually originates in an adjacent
hospital emergency department.Analysis of pooled data at this
3.2.7 Regional Emergency Medical Services Organization
level facilitates medical quality assurance activities and mini-
(REMSO)—Political users of the EMS-MIS at the regional
mizes the necessity for uploading confidential and sensitive
level. This could include an organizational entity such as a
data to higher levels of the pyramid.
regional EMS council, a multi-county hospital consortium, and
so forth, or a regional coordinating division within the prevail- 4.6.3 Access to hospital in-patient data may occur at the
ing EMS authority.
hospital or state level. More rapid feedback to medical care
providers is possible when the in-patient data are accessed
4. Summary of Guide while the patient is hospitalized or shortly after discharge.
Statewide hospital data are usually merged and available
4.1 The ability to deliver high-quality, cost-effective pre-
within six months after the year’s end. These state data are
hospital care can be enhanced by analysis of information about
useful for planning and for linkage to nonmedical data.
theEMSsystem’sstructure,process,andoutcomes.Thisguide
4.6.4 Laptop/palmtop and other computer technology that
defines a standardized terminology and recommends a concep-
permits computerized data entry at the scene facilitates imme-
tual design for a computerized EMS-MIS which can facilitate
diate and efficient access to the data by local EMS-MIS in
such analysis.
addition to timely export to regional and statewide entities.
4.2 This guide is intended to serve as a blueprint for the
4.7 All data element definitions, formats, and data commu-
initiation of such a system in geopolitical areas where comput-
nications protocols herein will be coordinated with those of the
erized EMS-MIS is not available or is being updated and to
ASTM E31.12 Subcommittee on the Computerized Patient
provide a standard basis for data collection to allow for
Record, the Center for Disease Control Consensus Trauma
meaningfulcomparisonsbetweenEMSsystemsthroughoutthe
Registry Minimum Data Set, the NHTSA uniform prehospital
country. The EMS-MIS’s already in operation should give
EMS data elements, and the Subcommittee on Ambulatory
serious consideration to restructuring their databases to be
Care Statistics and the InteragencyTask Forces of the National
consistent with this guide.
Committee on Vital and Health Statistics for the Uniform
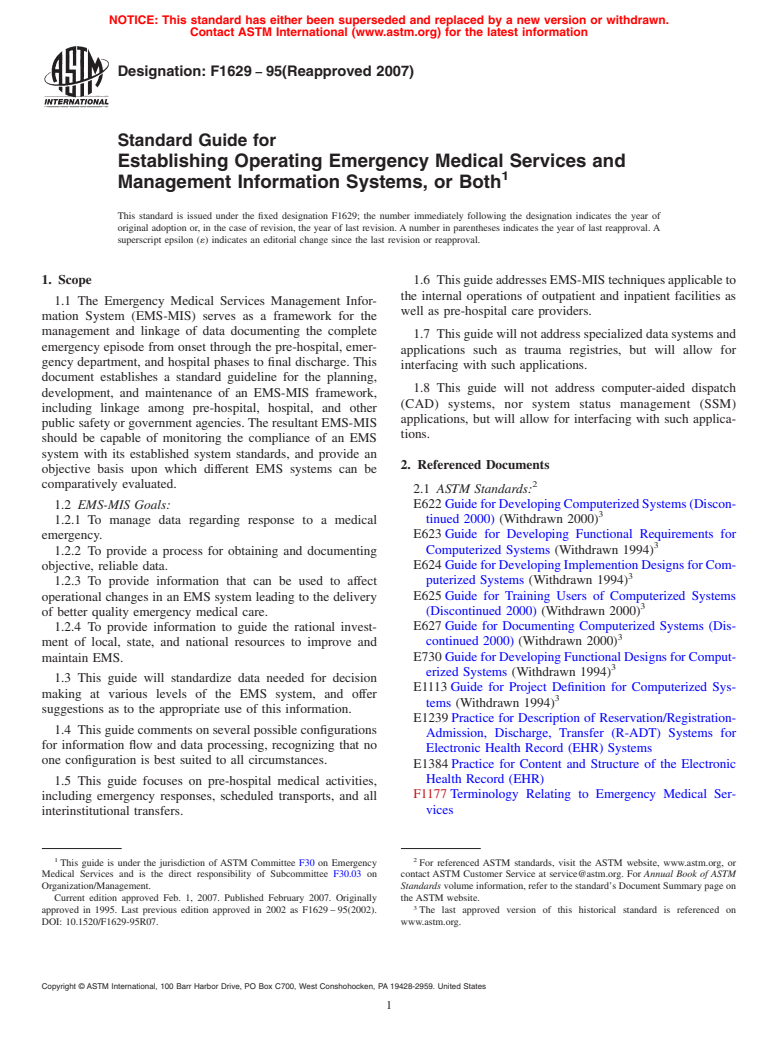
4.3 Fig. 1 defines the major organizational entities involved
AmbulatoryCareDataSetandtheUniformHospitalDischarge
in day-to-day EMS operations. This diagram is based upon the
Data Set.
assumption that these organizations represent the potential
sources of all data and policies needed for the EMS-MIS. It 4.8 The EMS-MIS’s may wish to include additional data
shows types of data and reports available from the various elements in their databases for a variety of purposes. In
entities, and needed by them to optimize their operation. addition to the sources listed in 4.7, some of the data elements
F1629 − 95 (2007)
FIG. 1 EMS-MIS Context Diagram I
presented in 5.3 were chosen if they met either of the 4.9.3 The logical database file the element should reside in.
conditions listed as follows: (See 5.8.6.7 for the list of database files.)
4.8.1 The data element is necessary for identification/ 4.9.4 The organizations that should have possession of the
documentation or recall/linkage of the event, or both.
element routinely and optionally.
4.8.2 The data element is needed for generation of a useful
4.9.5 Those who should have access to the element.
management report.
4.9.6 The purpose of the data element and its various uses.
4.9 The data list was kept as small as feasible for reasons of
4.10 After review of the information in 4.9.1 to 4.9.6, the
practicality, cost, and a better chance of successful implemen-
task group will vote to include/exclude the element, and so
tation of the system as a whole. It reflects the consensus of the
advise Subcommittee F30.03.
Task Group and the 1994 national consensus conference
4.11 Certain key identifiers must exist in a planned, coordi-
sponsored by the National Highway Traffic SafetyAdministra-
nated manner in order for an EMS-MIS to function efficiently
tion.Additions to the standard data set herein will be made by
and without ambiguity. There should be a system in each state
the following procedure: Any person who proposes a data
that allows for the assignment of unique identification or
element for inclusion in the data set should submit the
registration numbers to each of the following:
following information, in writing, to the F30.03.03 Task
4.11.1 Individual providers.
Group.
4.11.2 Provider service organizations (PSO).
4.9.1 An explicit definition of the element.
4.9.2 The organization in the Level I Context Diagram (Fig. 4.11.3 Individual vehicles owned or operated by PSO’s, or
1) responsible for recording the data element. both.
F1629 − 95 (2007)
FIG. 2 EMS-MIS Context Diagram II
4.11.4 First responder organizations. scope of information to be elicited during a given patient
4.11.5 Physicians. encounter. These data elements should, however, be docu-
4.11.6 Nurses.
mented and subsequently computerized for generation of
4.11.7 Hospitals.
management reports.
4.11.8 Non-hospital in-patient institutions (nursing homes,
5.2 Identification of Sources of Data—Data for the EMS-
rehabilitation facilities, and so forth).
MIS should be collected from the source organizations listed
4.11.9 Astatewide,standard,patientcarerecord.Therecord
andshowninFig.1andFig.2.Theresponsibilityforcollecting
may be computerized, or paper, or both. Regardless of the
the data should rest with the organization as detailed. Respon-
form, the record should be prenumbered or assigned a unique
sibility for computerizing the data depend upon the specifics of
identifier on a real-time basis.
the individual EMS-MIS design (see 5.8).
5. Significance and Use
5.2.1 Provider Organization Patient Care Records (PCR),
(Run Reports):
5.1 Data recorded during the patient’s pre-hospital phase of
care should become a part of the patient’s formal emergency 5.2.1.1 Each provider organization should document every
time a vehicle is dispatched regardless of the outcome of the
department or inpatient medical record, or both. The data
elementslistedhereinarenotmeanttolimitordefinetheentire call.
F1629 − 95 (2007)
5.2.1.2 Separate PCR’s must be completed by each PSO for 5.3.2.4 *Time Incident Reported—Time the call is first
every patient who is treated or transported, or both. Each received by a public safety answering point (PSAP) or other
patient must be identified by a record number that is unique designated entity.
statewide.
5.3.2.5 •Public Safety Incident Number—The incident num-
5.2.1.3 Patient care records should be computerized at the
ber assigned by the PSAP when the call for help is received.
local level whenever feasible to promote efficient data access.
5.3.2.6 *Time EMS Dispatch Notified—Time of first con-
5.2.1.4 PCR’s should include the applicable data elements
nection with EMS dispatch.
as defined in 5.3.2.
5.3.2.7 *Incident Number—Unique number for each inci-
5.2.1.5 A process for obtaining the data elements collected
dent reported to EMS dispatch. Thi
...






Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.