ISO/PAS 7020:2023
(Main)Sizing parameters of surgical valve prostheses: Requirements regarding the application of ISO 5840-2
Sizing parameters of surgical valve prostheses: Requirements regarding the application of ISO 5840-2
This document describes in vitro methods of measurement of the sizing parameters for surgical valves (referring to mechanical and stented bioprosthetic valves only here and hereafter). It represents a consensus reached among manufacturers, independent bioengineers and clinicians, and is underpinned by interlaboratory studies. This document relates to surgical heart valve prostheses and is intended to be used in conjunction with ISO 5840-1:2021 and ISO 5840-2:2021. Where noted, the requirements of this document clarify certain requirements of ISO 5840-1 and/or ISO 5840-2. Specific methodologies are included for flexible leaflet (bioprosthetic) and rigid (mechanical) valves. Sutureless valves, stentless valves and valved conduits are not included.
Désignation des dimensions des prothèses valvulaires chirurgicales: Exigences relatives à l'application de l'ISO 5840-2
General Information
Standards Content (Sample)
PUBLICLY ISO/PAS
AVAILABLE 7020
SPECIFICATION
First edition
2023-05
Sizing parameters of surgical valve
prostheses: Requirements regarding
the application of ISO 5840-2
Désignation des dimensions des prothèses valvulaires chirurgicales:
Exigences relatives à l'application de l'ISO 5840-2
Reference number
© ISO 2023
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on
the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address below
or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii
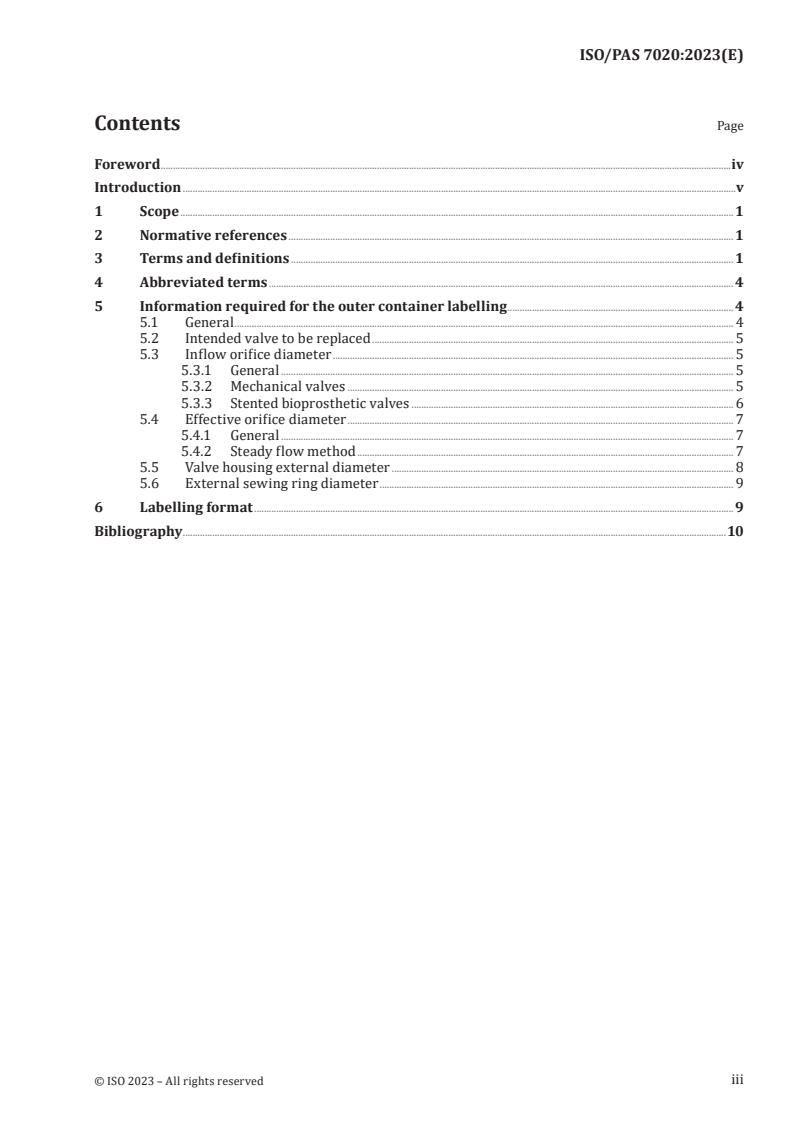
Contents Page
Foreword .iv
Introduction .v
1 Scope . 1
2 Normative references . 1
3 Terms and definitions . 1
4 Abbreviated terms . 4
5 Information required for the outer container labelling . 4
5.1 General . 4
5.2 Intended valve to be replaced . 5
5.3 Inflow orifice diameter . 5
5.3.1 General . 5
5.3.2 Mechanical valves . 5
5.3.3 Stented bioprosthetic valves . 6
5.4 Effective orifice diameter . 7
5.4.1 General . 7
5.4.2 Steady flow method . 7
5.5 Valve housing external diameter . 8
5.6 External sewing ring diameter . 9
6 Labelling format .9
Bibliography .10
iii
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out
through ISO technical committees. Each member body interested in a subject for which a technical
committee has been established has the right to be represented on that committee. International
organizations, governmental and non-governmental, in liaison with ISO, also take part in the work.
ISO collaborates closely with the International Electrotechnical Commission (IEC) on all matters of
electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are
described in the ISO/IEC Directives, Part 1. In particular, the different approval criteria needed for the
different types of ISO document should be noted. This document was drafted in accordance with the
editorial rules of the ISO/IEC Directives, Part 2 (see www.iso.org/directives).
ISO draws attention to the possibility that the implementation of this document may involve the use
of (a) patent(s). ISO takes no position concerning the evidence, validity or applicability of any claimed
patent rights in respect thereof. As of the date of publication of this document, ISO had not received
notice of (a) patent(s) which may be required to implement this document. However, implementers are
cautioned that this may not represent the latest information, which may be obtained from the patent
database available at www.iso.org/patents. ISO shall not be held responsible for identifying any or all
such patent rights.
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation of the voluntary nature of standards, the meaning of ISO specific terms and
expressions related to conformity assessment, as well as information about ISO's adherence to
the World Trade Organization (WTO) principles in the Technical Barriers to Trade (TBT), see
www.iso.org/iso/foreword.html.
This document was prepared by Technical Committee ISO/TC 150, Implants for surgery, Subcommittee
SC 2, Cardiovascular implants and extracorporeal systems.
Any feedback or questions on this document should be directed to the user’s national standards body. A
complete listing of these bodies can be found at www.iso.org/members.html.
iv
Introduction
0.1 General
In the past, inconsistencies have been reported with the labelling and instructions for use associated
with sizing parameters and sizing procedures for surgical replacement heart valves, specifically,
mechanical and stented bioprosthetic valves. These inconsistencies have led to confusion among
some users about which size valve to implant in a particular patient and have also led to challenges in
comparing results (published or otherwise) from one valve model to another. A solution to the problem
can be achieved by providing more complete and accurate sizing information to the clinicians, which
will ultimately benefit the patients.
ISO 5840-2 identifies a number of sizing parameters that are required in the labelling (including on the
unit box, see ISO 5840-2:2021, 6.3.3, and instructions for use) to inform the selection of a surgical heart
valve prosthesis to be implanted in a specific patient. However, no guidance is offered in ISO 5840-2 on
how these parameters should be obtained.
0.2 Clinical rationale for additional sizing information
Successful valve replacement therapy requires that an adequate size surgical heart valve substitute is
used, based on patient body size and the native valve annulus size. An understanding of valve sizing
parameters and appropriate choice of size is critical to post-procedure success since a valve substitute
that is too small for the patient can result in prosthesis-patient mismatch. For aortic valve replacements,
[1]
severe mismatch has been reported in 5 % to 15 % of patients. Severe prosthesis-patient mismatch
leads to increased early, mid-term and late mortality, especially if the left ventricular ejection fraction
[2]-[5] [5]
(LVEF) is reduced. In the mid-term, it causes a higher incidence of heart failure and limits left
[5]
ventricular mass regression. In the long term, it can also contribute to accelerated structural valve
[6]
degeneration (SVD). Patients with severe prosthesis-patient mismatch can require replacement of
the valve substitute with another having a larger effective orifice area (EOA). However, re-intervention
has significant risk of mortality and morbidity.
The best approach to prosthesis-patient mismatch is prevention. This requires the surgeon to have
clear and accurate information about the sizing parameters and EOA of each valve substitute.
A surgical heart valve substitute is described by a labelled size given by the manufacturer, which is
assumed to be broadly consistent with the size of the patient native valve annulus for which the valve
[1]
is intended. Literature reviews and studies of haemodynamic function commonly compare valve
substitutes by labelled size, but there can be major differences between the patient native valve annulus
[8]-[11]
diameter and the labelled size of the valve substitute. Intraoperative sizing is further complicated
by the need for aortic supra-annular valves to fit within the aortic sinus. The disparity between labelled
size and actual size means that echocardiographic or clinical comparisons based on labelled size can be
misleading.
The issue of valve sizing is a complex problem and is being addressed in a stepwise fashion. The working
group revising ISO 5840-2 proposed a first step toward greater transparency by requiring additional
information be added to the unit box, namely, internal orifice diameter and effective orifice diameter.
Although this information does not necessarily inform the surgeon on whether the valve would fit in
the patient’s annulus, it helps to estimate the internal orifice available for blood flow and thus indirectly
the EOA. It is not feasible to use clinically measured EOA’s since sizing information must be available
before a surgical heart valve substitute is released for use in patients. Indeed, it can take a number of
years to gather sufficient echocardiographic data to confirm the clinical EOAs. Furthermore, the use
of echocardiographic data to help avoid prosthesis-patient mismatch has been criticized because of
[12]
variability in the measurements obtained in vivo. In vitro steady flow data have less variability and
allow meaningful comparison of every design and size of surgical heart valve substitute under the same
flow conditions. This information can be used by the surgeon to choose a specific valve substitute type
and size based on more standardized parameters than labelled valve size. It is anticipated that further
steps toward a standardised approach to sizing will be addressed in subsequent editions of ISO 5840-2.
v
This document provides further specifications to explain these two parameters (i.e. internal orifice
diameter and effective orifice diameter) and other sizing parameters. This document also guides the
manufacturer in selecting reproducible methods to obtain these parameters and the degree of accuracy
required.
vi
PUBLICLY AVAILABLE SPECIFICATION ISO/PAS 7020:2023(E)
Sizing parameters of surgical valve prostheses:
Requirements regarding the application of ISO 5840-2
1 Scope
This document describes in vitro methods of measurement of the sizing parameters for surgical valves
(referring to mechanical and stented bioprosthetic valves only here and hereafter). It represents a
consensus reached among manufacturers, independent bioengineers and clinicians, and is underpinned
by interlaboratory studies.
This document relates to surgical heart valve prostheses and is intended to be used in conjunction with
ISO 5840-1:2021 and ISO 5840-2:2021. Where noted, the requirements of this document clarify certain
requirements of ISO 5840-1 and/or ISO 5840-2. Specific methodologies are included for flexible leaflet
(bioprosthetic) and rigid (mechanical) valves. Sutureless valves, stentless valves and valved conduits
are not included.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
ISO 5840-1:2021, Cardiovascular implants — Cardiac valve prostheses — Part 1: General requirements
ISO 5840-2:2021, Cardiovascular implants — Cardiac valve prostheses — Part 2: Surgically implanted
heart valve substitutes
3 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminology databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https:// www .iso .org/ obp
— IEC Electropedia: available at https:// www .electropedia .org/
3.1
effective orifice area
EOA
A
eo
orifice area that has been derived from flow and pressure or velocity data
Note 1 to entry: For in vitro testing, EOA is defined as:
q
V
RMS
A =
eo
Δp
51,6
ρ
where
A
is the effective orifice area, expressed in cm ;
eo
q
is the root mean square forward flow, expressed in ml/s, during the positive differential
V
RMS
pressure period;
Δp
is the mean pressure difference, expressed in mmHg;
ρ 3
is the density of the test fluid, expressed in g/cm .
3.2
external sewing ring diameter
ESRD
OD-SEWINGRING
outside diameter of the sewing ring at the largest point
Note 1 to entry: The external sewing ring diameter is expressed in millimetres.
Note 2 to entry: See Figure 1.
3.3
heart valve substitute
device used to replace the function of a native valve of the heart
3.4
inflow orifice diameter
ID-INFLOW
inflow internal orifice diameter
orifice diameter measured at inflow with a validated procedure
Note 1 to entry: See Figure 1.
Note 2 to entry: This definition clarifies the definition ISO 5840-2:2021, 3.5 for prosthesis minimum internal
diameter for a flexible surgical heart valve.
3.5
inflow orifice diameter
ID-INFLOW
inflow internal orifice diameter
inner diameter of the valve housing
Note 1 to entry: See Figure 1.
Note 2 to entry: This definition clarifies the definition ISO 5840-2:2021, 3.6 for prosthesis minimum internal
diameter for a rigid surgical heart valve.
3.6
intra-annular
wholly or partially within the patient’s annulus
Note 1 to entry: See Figure 1.
Key
1 inflow orifice diameter
2 patient annulus diameter
3 external sewing ring diameter
A aortic/pulmonic intra-annular
B aortic/pulmonic supra-annular
C mitral/tricuspid intra-annular
NOTE This figure is a clarification of ISO 5840-2:2021, Figure 1.
Figure 1 — Designation of dimensions of surgical heart valve substitute sewing ring
configurations
3.7
occluder
leaflet component that inhibits backflow
3.8
patient annulus diameter
PAD
diameter of the smallest flow area within the patient’s valve annulus
Note 1 to entry: PAD is expressed in millimetres.
Note 2 to entry: See Figure 1.
3.9
effective orifice diameter
ID-EFFECTIVE
D
eff
prosthesis minimum internal diameter
diameter derived from hydrodynamic performance data measured with a standard validated procedure
Note 1 to entry: This definition clarifies the definition ISO 5840-2:2021, 3.5 for prosthesis minimum internal
diameter.
Note 2 to entry: The effective orifice diameter, D , is calculated from EOA data as
eff
A
eo
D = 2
eff
π
where A is the EOA derived from the steady flow pressure gradient.
eo
3.10
supra-annular
wholly above the patient’s annulus
Note 1 to entry: See Figure 1.
3.11
valve housing external diameter
OD-HOUSING
outer diameter of the structure that houses the prosthetic valve leaflets
3.12
valve size
designated valve size
manufacturer's designation of a surgical heart valve substitute which indicates the intended patient
annulus diameter
Note 1 to entry: The valve size equals to the patient annulus diameter (3.9).
Note 2 to entry: This takes into consideration the manufacturer's recommended implant position relative to the
annulus and the suture technique.
4 Abbreviated terms
EOA effective orifice area
ESRD external sewing ring diameter
ID-INFLOW inflow orifice diameter
ID-EFFECTIVE effective orifice diameter
LVEF left ventricular ejection fraction
OD-HOUSING outer diameter of housing or valve stent
OD-SEWINGRING sewing ring external diameter
PAD patient annulus diameter
SVD structural valve deterioration
5 Information required for the outer container labelling
5.1 General
ISO 5840-2:2021, 6.3.3 specifies packaging, labelling and sterilization requirements for surgical heart
valve prostheses. Most requirements are referenced to ISO 5840-2:2021, 6.3.3. However, ISO 5840-2
includes some additional labelling requirements to appear on the “outer container labelling … in
diagrammatic and/or tabular form.” The additional items required are:
— intended valve to be replaced;
— intended position in relation to the annulus;
— inflow orifice diameter (see 3.4 and 3.5);
— effective orifice diameter (see 3.9);
— external sewing ring diameter (see 3.2).
-----
...







Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...