ASTM E2721-10
(Test Method)Standard Test Method for Evaluation of Effectiveness of Decontamination Procedures for Surfaces When Challenged with Droplets Containing Human Pathogenic Viruses
Standard Test Method for Evaluation of Effectiveness of Decontamination Procedures for Surfaces When Challenged with Droplets Containing Human Pathogenic Viruses
SIGNIFICANCE AND USE
The efficacy of disinfection technologies can be evaluated on finished products, as well as on developmental items.
This test method defines procedures for validation of the droplet generator, preparation of the test specimen, application of the challenge virus, enumeration of viable viruses, assessing data quality, and calculation of decontamination efficiency.
This test method provides defined procedures for creating droplets that approximate those produced by human respiratory secretions, with particular emphasis on droplet size distribution and aerosolization media.
Safety concerns associated with aerosolizing microbial agents are not addressed as part of this test method. Individual users should consult with their local safety authority, and a detailed biological aerosol safety plan and risk assessment should be conducted prior to using this method. Users are encouraged to consult the manual Biosafety in Microbiological and Biomedical Laboratories published by the U.S. Centers for Disease Control and Prevention (CDC).
This test method differs from Test Methods E1052 and E2197 in the presentation of virus to the surface. The aforementioned test methods use liquid inoculum to contaminate carrier surfaces, whereas this method presents the virus in droplets that are representative of human respiratory secretions
This method differs from Test Method , because (1) larger droplets are being formed, (2) the droplets will not be completely dried prior to application to surfaces, (3) the droplets can be applied to any surfaces, not just those that are air permeable, and (4) unique equipment is required to create droplets.
SCOPE
1.1 This test method is designed to evaluate decontamination methods (physical, chemical, self-decontaminating materials) when used on surfaces contaminated with virus-containing droplets.
1.2 This test method defines the conditions for simulating respiratory droplets produced by humans and depositing the droplets onto surfaces.
1.3 The method is specific to influenza viruses but could be adapted for work with other types of respiratory viruses or surrogates (Appendix X5).
1.4 This test method is suitable for working with a wide variety of environmental surfaces.
1.5 This test method does not address the performance of decontaminants against microbes expelled via blood splatter, vomit, or fecal contamination.
1.6 This test method should be performed only by those trained in bioaerosols, microbiology, or virology, or combinations thereof.
1.7 The values stated in SI units are to be regarded as standard. No other units of measurement are included in this standard.
1.8 This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety and health practices and determine the applicability of regulatory limitations prior to use.
General Information
Relations
Standards Content (Sample)
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Contact ASTM International (www.astm.org) for the latest information
Designation: E2721 − 10
StandardTest Method for
Evaluation of Effectiveness of Decontamination Procedures
for Surfaces When Challenged with Droplets Containing
Human Pathogenic Viruses
This standard is issued under the fixed designation E2721; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision.Anumber in parentheses indicates the year of last reapproval.A
superscript epsilon (´) indicates an editorial change since the last revision or reapproval.
INTRODUCTION
Many communicable diseases can often spread through droplets containing infectious agents. Such
“contagious droplets” may expose susceptible individuals directly or contaminate environmental
surfaces in the immediate vicinity and render them as fomites for further spread of the disease. The
characteristics of the droplets (particle size and composition) will influence the viability of the
microorganisms when exposed to environmental stresses but also shield them from physical and
chemical decontaminants. The wide variations in the types and levels of such protective/shielding
ingredients can impact on the effectiveness of surface decontaminants. This test method is designed
tosimulatesurfacedepositionofcontagiousdropletsfromhumanrespiratorysecretions.Itisprimarily
focused on influenza viruses but other respiratory viruses or surrogates could be used. Protocols for
assessing the microbicidal activity of disinfectants are also described.
1. Scope 1.7 The values stated in SI units are to be regarded as
standard. No other units of measurement are included in this
1.1 This test method is designed to evaluate decontamina-
standard.
tion methods (physical, chemical, self-decontaminating mate-
rials) when used on surfaces contaminated with virus-
1.8 This standard does not purport to address all of the
containing droplets. safety concerns, if any, associated with its use. It is the
responsibility of the user of this standard to establish appro-
1.2 This test method defines the conditions for simulating
priate safety and health practices and determine the applica-
respiratory droplets produced by humans and depositing the
bility of regulatory limitations prior to use.
droplets onto surfaces.
1.3 The method is specific to influenza viruses but could be
2. Referenced Documents
adapted for work with other types of respiratory viruses or
2.1 ASTM Standards:
surrogates (Appendix X5).
E1052Test Method to Assess the Activity of Microbicides
1.4 This test method is suitable for working with a wide
against Viruses in Suspension
variety of environmental surfaces.
E2197Quantitative Disk Carrier Test Method for Determin-
1.5 This test method does not address the performance of
ing Bactericidal, Virucidal, Fungicidal, Mycobactericidal,
decontaminants against microbes expelled via blood splatter,
and Sporicidal Activities of Chemicals
vomit, or fecal contamination.
E2720Test Method for Evaluation of Effectiveness of De-
contamination Procedures for Air-Permeable Materials
1.6 This test method should be performed only by those
when Challenged with Biological Aerosols Containing
trained in bioaerosols, microbiology, or virology, or combina-
Human Pathogenic Viruses
tions thereof.
This test method is under the jurisdiction of ASTM Committee E35 on
Pesticides, Antimicrobials, and Alternative Control Agents and is the direct For referenced ASTM standards, visit the ASTM website, www.astm.org, or
responsibility of Subcommittee E35.15 on Antimicrobial Agents. contact ASTM Customer Service at service@astm.org. For Annual Book of ASTM
Current edition approved Oct. 1, 2010. Published February 2011. DOI: 10.1520/ Standards volume information, refer to the standard’s Document Summary page on
E2721–10. the ASTM website.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959. United States
E2721 − 10
NOTE 2—Nonviable techniques for viral enumeration such as poly-
2.2 EPA Standards:
merase chain reaction (PCR) or hemagglutination cannot be used.
EPA600⁄4-84⁄013(N16) USEPA Manual of Methods for
Virology 4.1.4 The virucidal activity of the decontamination proce-
2.3 WHO Standards: dure is determined from the log difference in viability between
treated and test carriers.
WHO Manualon Animal Influenza Diagnosis and Surveil-
lance
5. Significance and Use
3. Terminology
5.1 The efficacy of disinfection technologies can be evalu-
ated on finished products, as well as on developmental items.
3.1 Definitions:
3.1.1 aerosol, n—a suspension of solid or liquid particles in
5.2 Thistestmethoddefinesproceduresforvalidationofthe
a gas medium.
droplet generator, preparation of the test specimen, application
3.1.2 biological aerosol, n—aerosol comprising particles of
ofthechallengevirus,enumerationofviableviruses,assessing
biological origin or activity which may affect living things data quality, and calculation of decontamination efficiency.
through infectivity, allergencity, toxicity, or pharmacological
5.3 This test method provides defined procedures for creat-
and other processes.
ing droplets that approximate those produced by human
3.1.3 contact transmission, n—infections caused by direct
respiratory secretions, with particular emphasis on droplet size
skin-to-skin contact or indirect contact with objects contami-
distribution and aerosolization media.
nated with pathogens.
5.4 Safety concerns associated with aerosolizing microbial
3.1.4 contagious respiratory droplet, n—respiratory secre-
agents are not addressed as part of this test method. Individual
tions containing infectious microorganisms that form large
users should consult with their local safety authority, and a
droplets (≥5 µm) and settle out of the air over short distances.
detailed biological aerosol safety plan and risk assessment
should be conducted prior to using this method. Users are
3.1.5 droplet transmission, n—direct transfer of pathogen-
containing droplets to conjuncitval or mucous membranes. encouragedtoconsultthemanual Biosafety in Microbiological
and Biomedical Laboratories published by the U.S. Centers
3.1.6 influenza, n—an infectious disease of birds and mam-
for Disease Control and Prevention (CDC).
mals caused by RNAviruses of the family Orthomyxoviridae.
5.5 This test method differs from Test Methods E1052 and
3.1.7 protective factor, n—soluble or insoluble material
E2197 in the presentation of virus to the surface. The afore-
co-deposited with microorganisms that directly protects the
mentioned test methods use liquid inoculum to contaminate
microorganism from environmental stresses or decontami-
carrier surfaces, whereas this method presents the virus in
nants.
dropletsthatarerepresentativeofhumanrespiratorysecretions
3.1.8 self-sanitizing material, n—a substrate containing an
5.6 This method differs from Test Method E2720, because
antimicrobial agent that collectively acts as a germicide.
(1)largerdropletsarebeingformed,(2)thedropletswillnotbe
4. Summary of Test Method
completely dried prior to application to surfaces, (3) the
droplets can be applied to any surfaces, not just those that are
4.1 The test method describes the steps required to deposit
air permeable, and (4) unique equipment is required to create
droplets onto surfaces and quantitatively assess decontamina-
droplets.
tion efficiency.
4.1.1 Using an aerosol device capable of meeting the data
6. Apparatus
quality objectives set for in this test method, influenza virus or
6.1 Droplet Apparatus—The apparatus used to load micro-
surrogates are aerosolized to form droplets that are subse-
organisms onto a substrate is composed of several commer-
quently applied to surfaces.
6,7,8
ciallyavailablecomponentsandcanbereadilyconstructed.
4.1.2 The virus-contaminated carriers are subjected to dis-
The overall design of the apparatus can take various forms and
infection protocols and incubated for the specified time and
can be fashioned in different dimensions while meeting the
conditions. Control samples are incubated under identical
validation requirements and data quality objectives listed
conditions but are not exposed to the disinfection protocols.
below. Appendix X1 contains the description of a prototypical
NOTE 1—Carriers with incorporated microbicides do not receive any
additional disinfection treatment.An untreated control is needed to assess
antimicrobial efficacy.
CDC-NIH, Biosafety in Microbiological and Biomedical Laboratories, 5th
Edition, U.S. Department of Health and Human Services, Washington, D.C., 2009.
4.1.3 Virus particles are eluted from the test and control
Vo, E., Rengasamy, S., Shaffer, R., “Development of aTest System to Evaluate
carriers and viability is assessed by 50% tissue culture
Decontamination Procedures for Viral Droplets on Respirators.” Applied and
infectious dose assay (log TCID ).
Environmental Microbiology, Vol 75, No. 23, 2009, pp. 7303–7309.
10 50
Woo,M.H.,Hsu,Y.M.,Wu,C.Y.,Heimbuch,B.K.,Wander,J.D.,“ADevice
for a Consistent and Controlled Delivery ofAerosolized Droplets Containing Viral
Available from United States Environmental Protection Agency (EPA), Ariel Agents Onto Surfaces.” Journal of Aerosol Science, Vol 41, 2010, pp. 941-952.
Rios Bldg., 1200 Pennsylvania Ave., NW, Washington, DC 20460, http:// Heimbuch B. K., Wallace, W. H., Kinney, K., Lumley, A. E., Wu, C-Y, Woo,
www.epa.gov. M-H, Wander, J. D., “APandemic Influenza Preparedness Study: Use of Energetic
Webster, R., Cox, N., Stohr, K. WHO Manual on Animal Influenza Diagnosis Methods to Decontaminate Filtering Facepiece Respirators Contaminated with
and Surveillance. World Health Organization, Department of Communicable Dis- H1N1 Aerosols and Droplets,” American Journal of Infection Control, 2010, DOI
ease Surveillance and Response. WHO/CDS/CDR/2002.5 Rev. 1. 10.1016/j.ajic.2010.07.004.
E2721 − 10
device that can be used to load droplets onto surfaces. viruses may be used, but conditions for propagation and
However, it is the responsibility of the user of this standard to enumeration are not provided in this method.
validate the performance of the device prior to use. 7.1.2 Madin–Darby Canine Kidney (MDCK) Cell Line,
6.1.1 Validation requirements and baseline testing. ATCC CRL-34.
6.1.1.1 Environmental Conditions—Generator must be ca- 7.1.3 Artificial Saliva, see Table 1 in section 6.1.1.4.
pable of delivering air with a relative humidity of 50 6 10%. 7.1.4 Minimal Essential Medium With Earle’s Balanced
6.1.1.2 Loading uniformity across the diameter of the test Salts (EMEM).
specimen is required to ensure the even distribution of the 7.1.5 Heat-Inactivated Fetal Bovine Serum (45 min at
droplets over the surface of the carrier.Astandard deviation of 56°C).
60.5 log TCID is desired. 7.1.6 Penicillin/Streptomycin,10000unitspenicillinand10
10 50
6.1.1.3 Sample-to-Sample Variation Objective—The vari- mg streptomycin per mL.
abilityofvirusloadingformultiplesamplesloadedforasingle 7.1.7 L-Glutamine, 200 mM in 0.85% NaCl.
test must have a standard deviation of 60.5 log TCID . 7.1.8 Crystal Violet.
10 50
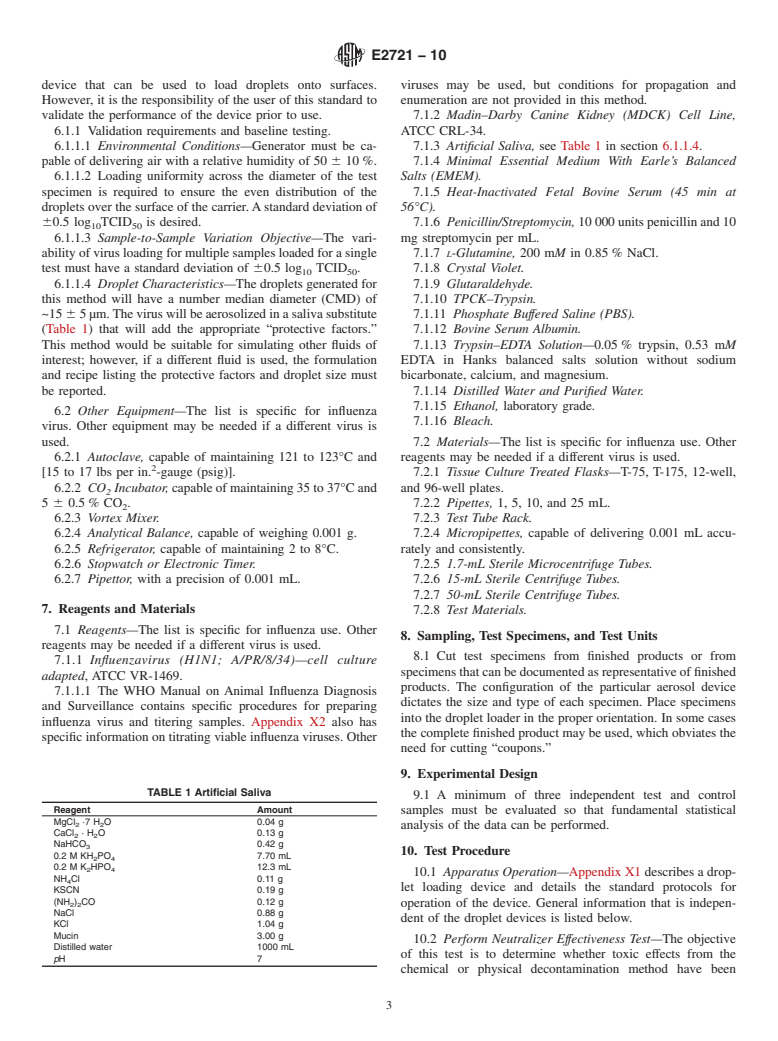
6.1.1.4 Droplet Characteristics—The droplets generated for 7.1.9 Glutaraldehyde.
this method will have a number median diameter (CMD) of 7.1.10 TPCK–Trypsin.
~15 65µm.Theviruswillbeaerosolizedinasalivasubstitute 7.1.11 Phosphate Buffered Saline (PBS).
(Table 1) that will add the appropriate “protective factors.” 7.1.12 Bovine Serum Albumin.
This method would be suitable for simulating other fluids of 7.1.13 Trypsin–EDTA Solution—0.05% trypsin, 0.53 mM
interest; however, if a different fluid is used, the formulation EDTA in Hanks balanced salts solution without sodium
and recipe listing the protective factors and droplet size must bicarbonate, calcium, and magnesium.
be reported. 7.1.14 Distilled Water and Purified Water.
7.1.15 Ethanol, laboratory grade.
6.2 Other Equipment—The list is specific for influenza
7.1.16 Bleach.
virus. Other equipment may be needed if a different virus is
used. 7.2 Materials—The list is specific for influenza use. Other
6.2.1 Autoclave, capable of maintaining 121 to 123°C and reagents may be needed if a different virus is used.
[15 to 17 lbs per in. -gauge (psig)]. 7.2.1 Tissue Culture Treated Flasks—T-75, T-175, 12-well,
6.2.2 CO Incubator,capableofmaintaining35to37°Cand and 96-well plates.
5 6 0.5% CO . 7.2.2 Pipettes, 1, 5, 10, and 25 mL.
6.2.3 Vortex Mixer. 7.2.3 Test Tube Rack.
6.2.4 Analytical Balance, capable of weighing 0.001 g. 7.2.4 Micropipettes, capable of delivering 0.001 mL accu-
6.2.5 Refrigerator, capable of maintaining 2 to 8°C. rately and consistently.
6.2.6 Stopwatch or Electronic Timer. 7.2.5 1.7-mL Sterile Microcentrifuge Tubes.
6.2.7 Pipettor, with a precision of 0.001 mL. 7.2.6 15-mL Sterile Centrifuge Tubes.
7.2.7 50-mL Sterile Centrifuge Tubes.
7. Reagents and Materials 7.2.8 Test Materials.
7.1 Reagents—The list is specific for influenza use. Other
8. Sampling, Test Specimens, and Test Units
reagents may be needed if a different virus is used.
8.1 Cut test specimens from finished products or from
7.1.1 Influenzavirus (H1N1; A/PR/8/34)—cell culture
specimensthatcanbedocumentedasrepresentativeoffinished
adapted, ATCC VR-1469.
products. The configuration of the particular aerosol device
7.1.1.1 The WHO Manual on Animal Influenza Diagnosis
dictates the size and type of each specimen. Place specimens
and Surveillance contains specific procedures for preparing
into the droplet loader in the proper orientation. In some cases
influenza virus and titering samples. Appendix X2 also has
the complete finished product may be used, which obviates the
specificinformationontitratingviableinfluenzaviruses.Other
need for cutting “coupons.”
9. Experimental Design
TABLE 1 Artificial Saliva
9.1 A minimum of three independent test and control
Reagent Amount
samples must be evaluated so that fundamental statistical
MgCl ·7 HO0.04g
2 2
analysis of the data can be performed.
CaCl ·HO0.13g
2 2
NaHCO 0.42 g
10. Test Procedure
0.2MKH PO 7.70 mL
2 4
0.2MK HPO 12.3 mL
2 4
10.1 Apparatus Operation—Appendix X1 describes a drop-
NH Cl 0.11 g
let loading device and details the standard protocols for
KSCN 0.19 g
(NH ) CO 0.12 g
2 2 operation of the device. General information that is indepen-
NaCl 0.88 g
dent of the droplet devices is listed below.
KCl 1.04 g
Mucin 3.00 g
10.2 Perform Neutralizer Effectiveness Test—The objective
Distilled water 1000 mL
of this test is to determine whether toxic effects from the
pH7
chemical or physical decontamination method have been
E2721 − 10
neutralized by the extraction buffer prior to virus enumeration. 11. Calculation or Interpretation of Results
...






Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.