ASTM F2502-05
(Specification)Standard Specification and Test Methods for Bioabsorbable Plates and Screws for Internal Fixation Implants
Standard Specification and Test Methods for Bioabsorbable Plates and Screws for Internal Fixation Implants
SIGNIFICANCE AND USE
Biodegradable devices are expected by intention to deteriorate over time once they are implanted into the body. This makes the removal operation obsolete, which is advantageous especially for pediatrics.
While the polymer degrades due to hydrolytic reaction with the environment, the mechanical performance of the device also deteriorates. The key to developing effective fracture fixation systems based on biodegradable devices is to provide an adequate level of fixation strength for a time frame that exceeds that expected for fracture healing. Once the fracture is healed, the device can be completely resorbed by the body.
Generally, biodegradable devices will be tested with similar test methods that are used to evaluate conventional metallic devices. In addition, one has to take into consideration the pre-test conditioning requirements, handling requirements, and time-dependent mechanical property evaluations for biodegradable devices.
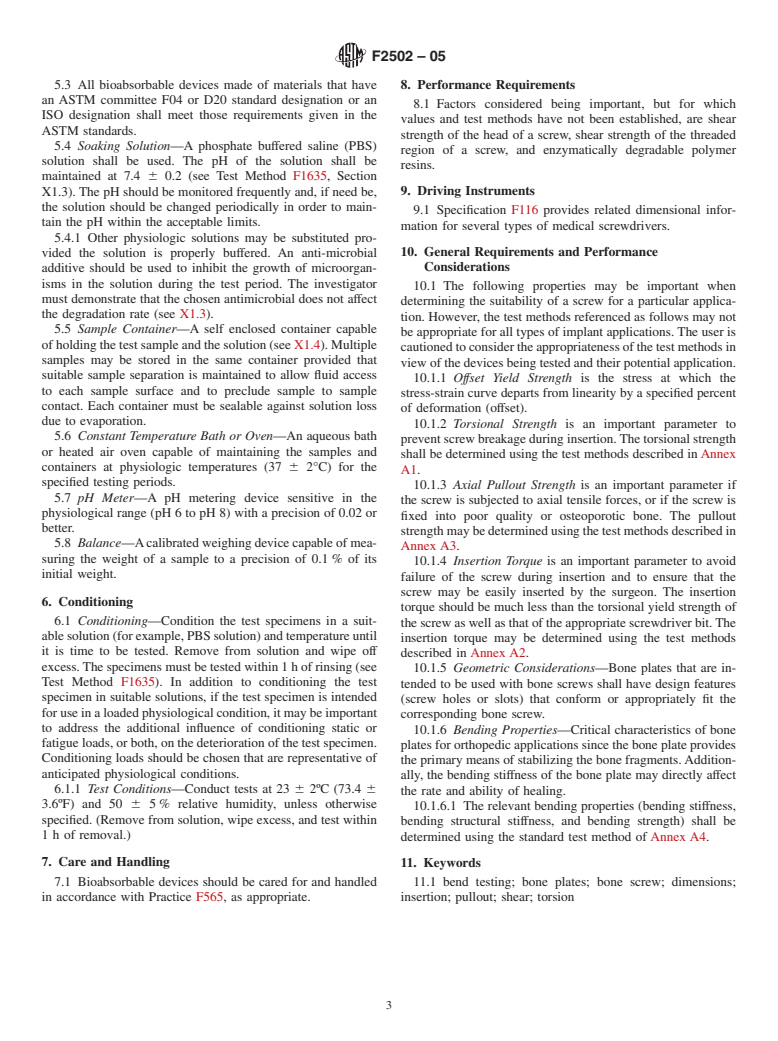
FIG. 1 Screw Parameters
SCOPE
1.1 This specification and test methods covers a mechanical characterization reference for hydrolytically degradable polymer resin (from this point on referenced as "bioabsorbable") plates and screws for orthopedic internal fixation.
1.2 This specification establishes common terminology to describe the size and other physical characteristics of bioabsorbable implants and performance definitions related to the performance of bioabsorbable devices.
1.3 This specification establishes standard test methods to consistently measure performance-related mechanical characteristics of bioabsorbable devices when tested under defined conditions of pretreatment, temperature, humidity, and testing machine speed.
1.4 This specification may not be appropriate for all bioabsorbable devices. The user is cautioned to consider the appropriateness of the standard in view of the particular bioabsorbable device and its potential application.
1.5 This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety and health practices and determine the applicability of regulatory limitations prior to use.
General Information
Relations
Standards Content (Sample)
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Contact ASTM International (www.astm.org) for the latest information.
Designation: F2502 – 05
Standard Specification and Test Methods for
Bioabsorbable Plates and Screws for Internal Fixation
Implants
This standard is issued under the fixed designation F2502; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (´) indicates an editorial change since the last revision or reapproval.
1. Scope With Specified Precision, the Average for a Characteristic
of a Lot or Process
1.1 This specification and test methods covers a mechanical
E1823 Terminology Relating to Fatigue and Fracture Test-
characterization reference for hydrolytically degradable poly-
ing
mer resin (from this point on referenced as “bioabsorbable”)
F116 Specification for Medical Screwdriver Bits
plates and screws for orthopedic internal fixation.
F382 Specification and Test Method for Metallic Bone
1.2 This specification establishes common terminology to
Plates
describe the size and other physical characteristics of bioab-
F543 Specification and Test Methods for Metallic Medical
sorbable implants and performance definitions related to the
Bone Screws
performance of bioabsorbable devices.
F565 Practice for Care and Handling of Orthopedic Im-
1.3 This specification establishes standard test methods to
plants and Instruments
consistently measure performance-related mechanical charac-
F1635 Test Method for in vitro Degradation Testing of
teristics of bioabsorbable devices when tested under defined
Hydrolytically Degradable Polymer Resins and Fabricated
conditions of pretreatment, temperature, humidity, and testing
Forms for Surgical Implants
machine speed.
F1839 Specification for Rigid Polyurethane Foam for Use
1.4 This specification may not be appropriate for all bioab-
as a Standard Material for Testing Orthopaedic Devices
sorbable devices. The user is cautioned to consider the appro-
and Instruments
priateness of the standard in view of the particular bioabsorb-
F1925 Specification for Semi-Crystalline Poly(lactide)
able device and its potential application.
Polymer and Copolymer Resins for Surgical Implants
1.5 This standard does not purport to address all of the
2.2 ISO Standards:
safety concerns, if any, associated with its use. It is the
ISO 13781 Poly (L-Lactide) Resins and Fabricated Forms
responsibility of the user of this standard to establish appro-
for Surgical Implants—In Vitro Degradation Testing
priate safety and health practices and determine the applica-
ISO 14630 Non-Active Surgical Implants—General Re-
bility of regulatory limitations prior to use.
quirements
2. Referenced Documents ISO 15814 Copolymers and Blends Based on
Polylactide—In Vitro Degradation Testing
2.1 ASTM Standards:
D790 Test Methods for Flexural Properties of Unreinforced
3. Terminology
and Reinforced Plastics and Electrical Insulating Materials
3.1 Definitions:
E4 Practices for Force Verification of Testing Machines
3.1.1 Unless otherwise defined in this specification, the
E6 TerminologyRelatingtoMethodsofMechanicalTesting
terminology related to mechanical testing that is used in these
E122 Practice for Calculating Sample Size to Estimate,
test methods will be in accordance with the definitions of
Terminologies E6 and E1823, and Specifications F382 and
F543.
This specification and test methods is under the jurisdiction of ASTM
3.2 General Definitions:
Committee F04 on Medical and Surgical Materials and Devices and is the direct
3.2.1 bioabsorbable device—a class of implants that are
responsibility of Subcommittee F04.21 on Osteosynthesis.
designed to deteriorate by means of biological resorption once
Current edition approved Oct. 1, 2005. Published October 2005. DOI: 10.1520/
F2502-05.
they are implanted into the body.
For referenced ASTM standards, visit the ASTM website, www.astm.org, or
contact ASTM Customer Service at service@astm.org. For Annual Book of ASTM
Standards volume information, refer to the standard’s Document Summary page on Available fromAmerican National Standards Institute (ANSI), 25 W. 43rd St.,
the ASTM website. 4th Floor, New York, NY 10036.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959, United States.
F2502 – 05
3.2.2 biological resorption—process by which degraded ment and fixation of two or more bone sections, primarily by
biomaterials(thatis,productsofdegradation)areeliminatedor spanning the fracture or defect.
incorporated, or both, by means of physiological metabolic
3.5.2 bone plate length, L (mm)—the linear dimension of
routes.
the bone plate measured along the longitudinal axis as illus-
3.2.3 deterioration (of a bioabsorbable device)—the action
trated in Fig. A4.2.
or process that results in a reduction of mass or mechanical
3.5.3 bone plate thickness, b (mm)—the linear dimension of
performance properties, or both.
the bone plate measured parallel to the screw hole axis as
3.2.4 hydrolytically degradable polymer (HDP)—any poly-
shown in Fig. A4.2. For a bone plate with a crescent section,
meric material in which the primary mechanism of chemical
the thickness is measured at the thickest point along the
degradation in the body is by hydrolysis (water reacting with
section.
the polymer resulting in cleavage of the chain).
3.5.4 bone plate width, w (mm)—thelineardimensionofthe
3.3 Definitions for Apparatus:
bone plate measured perpendicular to both the length and
3.3.1 data acquisition device—the data recorder shall be
thickness axes as shown in Fig. A4.2.
suitable to continuously record torque versus angle of rotation,
as well as linear displacement, calibrated in units of Newton-
4. Significance and Use
metres for torque and degrees for angle of rotation. The value
4.1 Biodegradable devices are expected by intention to
of torque shall have a resolution of 5 % of torsional yield
deteriorate over time once they are implanted into the body.
strength.Theangulardisplacementscaleshallhaveaminimum
This makes the removal operation obsolete, which is advanta-
sensitivity so as to enable an accurate offset measurement
geous especially for pediatrics.
capability for a 2° angular displacement (see A1.5.3).
4.2 While the polymer degrades due to hydrolytic reaction
3.3.2 pilot holes in test block—pilot holes shall be drilled in
with the environment, the mechanical performance of the
the test block for insertion and removal of the test specimen.
device also deteriorates. The key to developing effective
See Specification F543, Annex 2.
fracture fixation systems based on biodegradable devices is to
3.3.3 test block—the test block shall be fabricated from a
provide an adequate level of fixation strength for a time frame
uniform material that conforms to Specification F1839. See
that exceeds that expected for fracture healing. Once the
Specification F543, Annex 2.
fractureishealed,thedevicecanbecompletelyresorbedbythe
3.3.4 testing fixture—the torsion testing apparatus that is to
body.
be used for applying the required torque to the specimen shall
4.3 Generally, biodegradable devices will be tested with
be calibrated for the range of torques and rotational displace-
similar test methods that are used to evaluate conventional
ments used in the determination. A suitable testing fixture for
metallic devices. In addition, one has to take into consideration
the torsional yield strength-maximum torque-breaking angle
the pre-test conditioning requirements, handling requirements,
test is illustrated in Fig. A1.1.
and time-dependent mechanical property evaluations for bio-
3.3.5 test specimen—the test specimen shall be a com-
degradable devices.
pletely fabricated and finished bioabsorbable bone screw.
3.3.6 torque transducer—a transducer to translate the ap-
5. Materials and Manufacture
plied torque into an electrical signal amenable to continuous
recording, calibrated over the range of torques, both in the 5.1 Bioabsorbable devices may be fabricated from one of
clockwise and counterclockwise rotation, to be encountered in the following materials:
the test method, shall be provided.
5.1.1 l-lactide, d-lactide, d,l-lactide, glycolide, or other
3.3.7 torsional displacement transducer—a transducer to
known hydrolytically degradable polymer resins or copoly-
translate the angle of twist into an electrical signal amenable to
mers. (See ISO 13781, ISO 15814, Test Method F1635, and
continuous recording, calibrated over the range of angles to be Specification F1925.)
encountered in the test and an accuracy of 61 % of reading,
5.2 The manufacturer is responsible to ensure that materials
both in the clockwise and counterclockwise rotation, shall be
used to manufacture bioabsorbable implants are suitable for
used.
implanting into the body. Methods to evaluate a material’s
3.4 Definitions for Screw Testing:
suitability are described in ISO 14630.
3.4.1 anchor—a bioabsorbable device or a component of a
bioabsorbable device that provides the attachment to the bone.
3.4.2 bone anchor—a bioabsorbable device that provides a
means to attach soft tissue to bone with a suture.
3.4.3 insertion depth (mm)—the linear advancement of the
bioabsorbabledeviceintothetestblockmeasuredrelativetoits
seated position at the test block’s surface prior to testing.
3.5 Definitions for Plate Testing:
3.5.1 bone plate—a device with two or more holes or slots,
or both, and a cross section that consists of at least two
dimensions (width and thickness), which generally are not the
same in magnitude. The device is intended to provide align- FIG. 1 Screw Parameters
F2502 – 05
5.3 All bioabsorbable devices made of materials that have 8. Performance Requirements
an ASTM committee F04 or D20 standard designation or an
8.1 Factors considered being important, but for which
ISO designation shall meet those requirements given in the
values and test methods have not been established, are shear
ASTM standards.
strength of the head of a screw, shear strength of the threaded
5.4 Soaking Solution—A phosphate buffered saline (PBS)
region of a screw, and enzymatically degradable polymer
solution shall be used. The pH of the solution shall be
resins.
maintained at 7.4 6 0.2 (see Test Method F1635, Section
9. Driving Instruments
X1.3). The pH should be monitored frequently and, if need be,
the solution should be changed periodically in order to main-
9.1 Specification F116 provides related dimensional infor-
tain the pH within the acceptable limits.
mation for several types of medical screwdrivers.
5.4.1 Other physiologic solutions may be substituted pro-
10. General Requirements and Performance
vided the solution is properly buffered. An anti-microbial
Considerations
additive should be used to inhibit the growth of microorgan-
isms in the solution during the test period. The investigator
10.1 The following properties may be important when
must demonstrate that the chosen antimicrobial does not affect
determining the suitability of a screw for a particular applica-
the degradation rate (see X1.3).
tion. However, the test methods referenced as follows may not
5.5 Sample Container—A self enclosed container capable
be appropriate for all types of implant applications. The user is
ofholdingthetestsampleandthesolution(seeX1.4).Multiple
cautionedtoconsidertheappropriatenessofthetestmethodsin
samples may be stored in the same container provided that
view of the devices being tested and their potential application.
suitable sample separation is maintained to allow fluid access
10.1.1 Offset Yield Strength is the stress at which the
to each sample surface and to preclude sample to sample
stress-strain curve departs from linearity by a specified percent
contact. Each container must be sealable against solution loss
of deformation (offset).
due to evaporation.
10.1.2 Torsional Strength is an important parameter to
5.6 Constant Temperature Bath or Oven—An aqueous bath
preventscrewbreakageduringinsertion.Thetorsionalstrength
or heated air oven capable of maintaining the samples and
shall be determined using the test methods described inAnnex
containers at physiologic temperatures (37 6 2°C) for the
A1.
specified testing periods.
10.1.3 Axial Pullout Strength is an important parameter if
5.7 pH Meter—A pH metering device sensitive in the
the screw is subjected to axial tensile forces, or if the screw is
physiological range (pH 6 to pH 8) with a precision of 0.02 or
fixed into poor quality or osteoporotic bone. The pullout
better.
strengthmaybedeterminedusingthetestmethodsdescribedin
5.8 Balance—Acalibratedweighingdevicecapableofmea-
Annex A3.
suring the weight of a sample to a precision of 0.1 % of its
10.1.4 Insertion Torque is an important parameter to avoid
initial weight.
failure of the screw during insertion and to ensure that the
screw may be easily inserted by the surgeon. The insertion
6. Conditioning
torque should be much less than the torsional yield strength of
6.1 Conditioning—Condition the test specimens in a suit-
thescrewaswellasthatoftheappropriatescrewdriverbit.The
ablesolution(forexample,PBSsolution)andtemperatureuntil
insertion torque may be determined using the test methods
it is time to be tested. Remove from solution and wipe off
described in Annex A2.
excess.The specimens must be tested within1hof rinsing (see
10.1.5 Geometric Considerations—Bone plates that are in-
Test Method F1635). In addition to conditioning the test
tended to be used with bone screws shall have design features
specimen in suitable solutions, if the test specimen is intended
(screw holes or slots) that conform or appropriately fit the
foruseinaloadedphysiologicalcondition,itmaybeimportant
corresponding bone screw.
to address the additional influence of conditioning static or
10.1.6 Bending Properties—Critical characteristics of bone
fatigue loads, or both, on the deterioration of the test specimen.
plates for orthopedic applications since the bone plate provides
Conditioning loads should be chosen that are representative of
the primary means of stabilizing the bone fragments.Addition-
anticipated physiological conditions.
ally, the bending stiffness of the bone plate may directly affect
6.1.1 Test Conditions—Conduct tests at 23 6 2ºC (73.4 6
the rate and ability of healing.
3.6ºF) and 50 6 5 % relative humidity, unless otherwise
10.1.6.1 The relevant bending properties (bending stiffness,
specified. (Remove from solution, wipe excess, and test within
bending structural stiffness, and bending strength) shall be
1 h of removal.)
determined using the standard test method of Annex A4.
7. Care and Handling 11. Keywords
7.1 Bioabsorbable devices should be cared for and handled 11.1 bend testing; bone plates; bone screw; dimensions;
in accor
...






Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.