ASTM F2943-14(2019)
(Guide)Standard Guide for Presentation of End User Labeling Information for Musculoskeletal Implants
Standard Guide for Presentation of End User Labeling Information for Musculoskeletal Implants
SIGNIFICANCE AND USE
4.1 Implantable medical device labeling often results in a variety of label formats and information prioritization. This variability can be seen not only across different manufacturers but also across different implant types.3 At present label design and layout is developed by a given manufacturer and represents balancing internal needs (such as manufacturing, distribution, and marketing), regulatory requirements within various markets, and end user needs (as identified by individual manufacturers performing “voice of the consumer” feedback on their label designs).
4.2 At no fault to any given manufacturer, this process, along with the manner in which label information competes for available “real estate” on a package, often leads to variable prioritization of label information and highly variable label designs. The impact of this variability on patient care is not well documented within the published literature. An article from AAOS Now in 2009 described potential issues around label variability and gave anecdotal evidence of its impact.3
4.3 No published literature demonstrating a clear and conclusive impact on patient safety resulting from implant label variability was identified. Despite this lack of evidence, anecdotal observations and input from various involved individuals and organizations (surgeons, operating room nurses, hospital administrators, product representatives, and manufacturers) suggests a potential, although unproven, benefit for an increased standardization of implant labeling.
4.4 The authors of this guide believe it is important to highlight that no universally accepted method for validation of a label’s effectiveness exists. Current validation methods consist of varying methods of customer feedback on an existing label design using formal customer questionnaires, informal customer feedback through individual polling, and internal manufacturer-driven studies. The label recommendations presented within this guide have not been valida...
SCOPE
1.1 The goal of this guide is to recommend a universal label format (across manufacturers and various implants) of content and relative location of information necessary for final implant selection within an implant’s overall package labeling.
1.2 This guide recommends package labeling for musculoskeletal based implants individually processed and packaged with the intent of being opened at the point of use, typically in the operating room.
1.3 This guide identifies the necessary, “high priority” label content and recommendations for the layout and location of information for accurate implant identification by the end users in the operating room environment.
1.4 This goal is achieved by creating a partitioned, secondary area of an implant’s package label or a separate label to present this information uniformly.
1.5 The authors of this guide identified the competing needs of regulatory requirements, manufacturing/distribution, and implant identification. It is recognized through our task group’s efforts that, if a manufacturer elects to implement these recommendations, balancing these competing needs may necessitate changing a manufacturer’s internal processes, relabeling their entire inventory (either at a single point in time or over a defined time period), or accepting duplicate information on an implant’s package label. No additional compromises that would allow the primary goal of uniform implant label design across manufacturers were identified.
1.6 It is not the intent of this guide to limit or dictate overall package labeling content.
1.7 It is not the intent of this guide to supplant existing regulatory requirements (only to augment or complement existing regulatory label requirements).
1.8 The use or application of multiple languages is not prevented by this guide; however, use of more than one language is discouraged on the implant selection sublabel (ISSL) defined in this guide. The langua...
General Information
Relations
Standards Content (Sample)
This international standard was developed in accordance with internationally recognized principles on standardization established in the Decision on Principles for the
Development of International Standards, Guides and Recommendations issued by the World Trade Organization Technical Barriers to Trade (TBT) Committee.
Designation: F2943 − 14 (Reapproved 2019)
Standard Guide for
Presentation of End User Labeling Information for
Musculoskeletal Implants
This standard is issued under the fixed designation F2943; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (´) indicates an editorial change since the last revision or reapproval.
1. Scope language is discouraged on the implant selection sublabel
(ISSL) defined in this guide. The language of choice is left to
1.1 The goal of this guide is to recommend a universal label
the manufacturer and should be dictated by the end user and
format (across manufacturers and various implants) of content
regulatory requirements in the jurisdictions where the device is
and relative location of information necessary for final implant
marketed. International symbols should also be considered to
selection within an implant’s overall package labeling.
avoid the need for multiple ISSLs where possible.
1.2 This guide recommends package labeling for musculo-
1.9 Use and implementation of this guide is optional and at
skeletal based implants individually processed and packaged
the sole discretion of the implant’s manufacturer. It shall be
with the intent of being opened at the point of use, typically in
implemented with the following considerations:
the operating room.
1.9.1 The content and layout of any orthopedic implant
1.3 This guide identifies the necessary, “high priority” label
label should be influenced by risk management activities and
content and recommendations for the layout and location of
all label formats should be validated.
information for accurate implant identification by the end users
1.9.2 If internal risk management activities recommend
in the operating room environment.
deviation from this guide, the manufacturer is discouraged
1.4 This goal is achieved by creating a partitioned, second- from implementing a hybrid label that partially applies the
principles and recommendations in this guide.
ary area of an implant’s package label or a separate label to
present this information uniformly.
1.10 The values stated in SI units are to be regarded as
standard. No other units of measurement are included in this
1.5 The authors of this guide identified the competing needs
of regulatory requirements, manufacturing/distribution, and standard.
implantidentification.Itisrecognizedthroughourtaskgroup’s
1.11 This standard does not purport to address all of the
efforts that, if a manufacturer elects to implement these
safety concerns, if any, associated with its use. It is the
recommendations, balancing these competing needs may ne-
responsibility of the user of this standard to establish appro-
cessitate changing a manufacturer’s internal processes, relabel-
priate safety, health, and environmental practices and deter-
ing their entire inventory (either at a single point in time or
mine the applicability of regulatory limitations prior to use.
over a defined time period), or accepting duplicate information
1.12 This international standard was developed in accor-
on an implant’s package label. No additional compromises that
dance with internationally recognized principles on standard-
would allow the primary goal of uniform implant label design
ization established in the Decision on Principles for the
across manufacturers were identified.
Development of International Standards, Guides and Recom-
mendations issued by the World Trade Organization Technical
1.6 It is not the intent of this guide to limit or dictate overall
Barriers to Trade (TBT) Committee.
package labeling content.
1.7 It is not the intent of this guide to supplant existing
2. Referenced Documents
regulatory requirements (only to augment or complement
2.1 ISO Standards:
existing regulatory label requirements).
ISO 13485 Medical Devices—Quality Management
1.8 The use or application of multiple languages is not
Systems—Requirements for Regulatory Purposes
prevented by this guide; however, use of more than one
ISO 15223–1 Medical Devices—Symbols to be Used with
Medical Device Labels, Labeling and Information to be
This guide is under the jurisdiction of ASTM Committee F04 on Medical and
Supplied—Part 1: General Requirements
Surgical Materials and Devices and is the direct responsibility of Subcommittee
F04.22 on Arthroplasty.
Current edition approved Aug. 15, 2019. Published August 2019. Originally
approved in 2013. Last previous edition approved in 2014 as F2943 – 14. DOI: Available fromAmerican National Standards Institute (ANSI), 25 W. 43rd St.,
10.1520/F2943-14R19. 4th Floor, New York, NY 10036, http://www.ansi.org.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959. United States
F2943 − 14 (2019)
3. Terminology 3.1.7 high-priority information, n—subset of information
required on the product labeling that is necessary for accurate
3.1 Definitions:
identification of the implant for use in the operating room
3.1.1 body side, adj—implantsthatareright/leftspecificand
environment.
for which side of the body they are intended.
3.1.1.1 Discussion—This may also include identifiers for 3.1.8 implant, n—implantablemedicaldeviceintendedtobe
totally or partially introduced into the human body or a natural
medial/lateral or anterior/posterior.
orifice, or to replace an epithelial surface or the surface of the
3.1.2 company, n—the business that is primarily responsible
eye, by surgical intervention, which is intended to remain in
for providing the product to the end user.
place for at least 30 days after the procedure, and which can
3.1.2.1 Discussion—It is preferred that this is reflective of
only be removed by medical or surgical intervention.
the company designation that will be commonly used by the
3.1.8.1 Discussion—This definition applies to implantable
end user to identify the implant.
medical devices other than active implantable medical devices
3.1.3 end of the box (EOB), n—the surface of an implant’s
(“implantable medical device” definition from ISO 13485,
packaging that is most commonly visible when the product is
Subclause 3.5).
placed in inventory/storage (see Fig. 1).
3.1.9 implant description, n—brief, generic description us-
3.1.3.1 Discussion—In the event a pouch is used instead of
ing terminology comprehensible by all end users regardless of
a box, this would be the most often visualized surface of the
her/his technical knowledge of the implant.
package. It is often the same surface used for identification and
selection of the implant by the end users and attempts to
3.1.10 implant selection sublabel (ISSL), n—subset of the
balance the competing needs of regulation, manufacturing,
primary label that is intended to augment/supplement the
distribution, and implant selection.
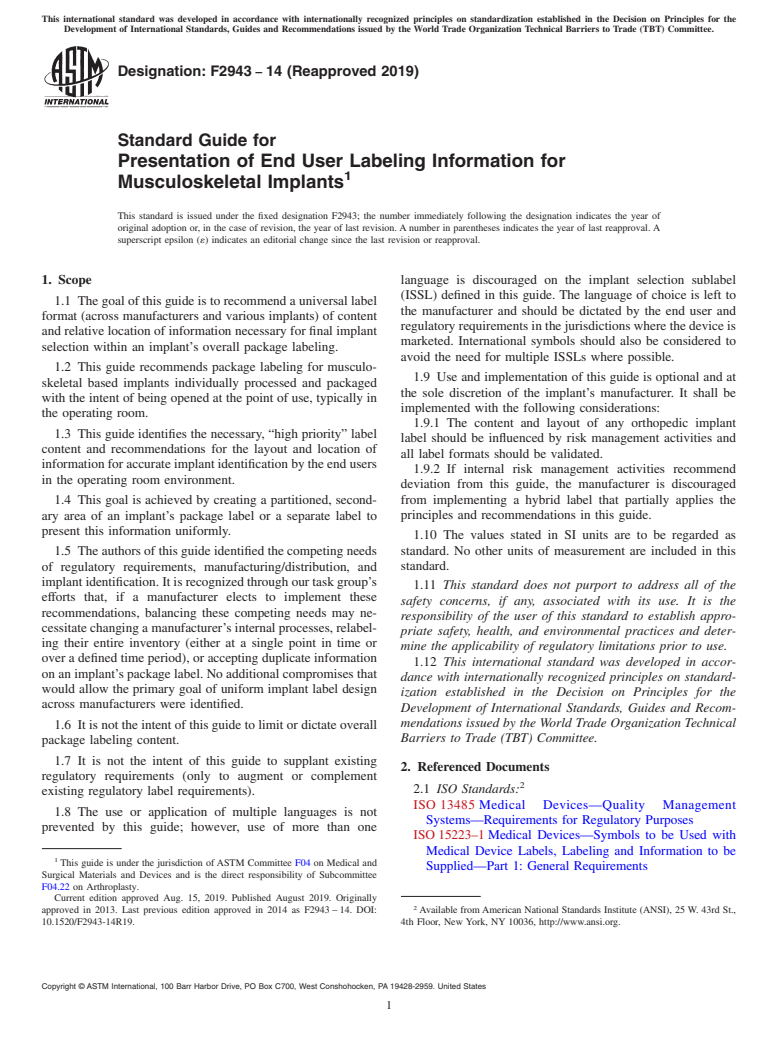
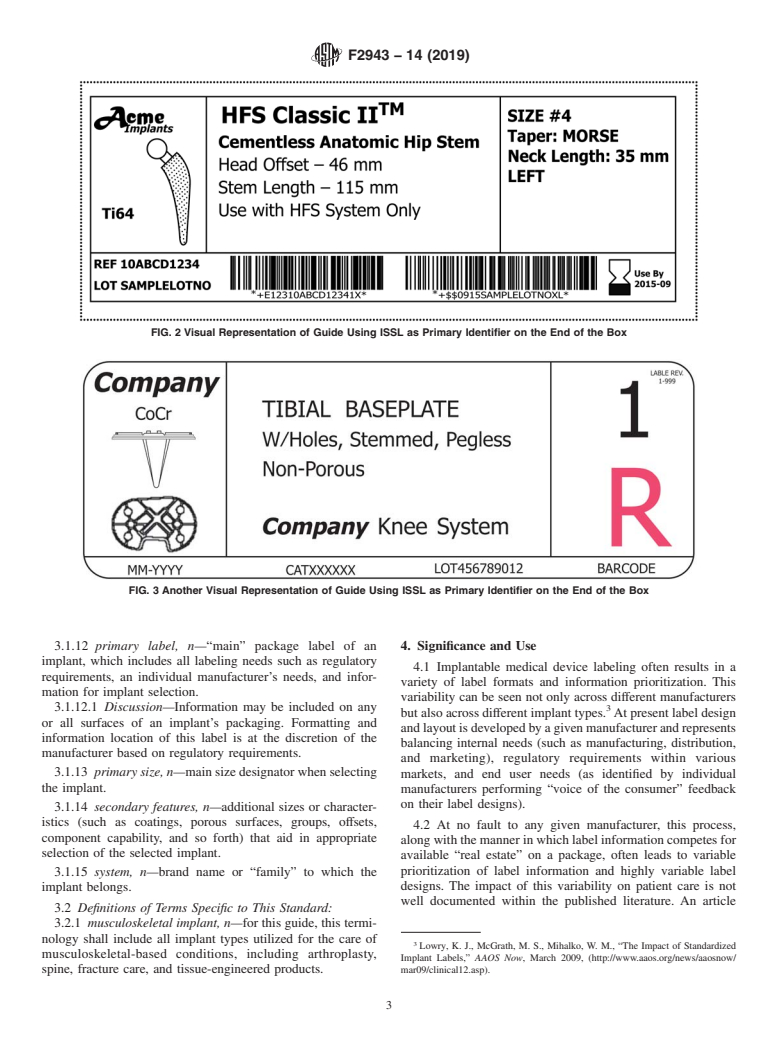
primary label (see examples in Fig. 2, Fig. 3, and Fig. 4).
3.1.4 end users, n—individuals who participate in the act of
3.1.10.1 Discussion—This area of the label shall include the
selecting the requested implant from inventory for final im-
necessary information for final implant selection presented in a
plantation in a patient; these include, but are not limited to, the
clear, uncluttered manner and is the only focus of this guide.
treating surgeon, operating room nurse, and operating room
3.1.11 package labeling, n—written, printed, or graphic
technician.
matter affixed to a medical device or any of its containers or
3.1.5 fold, n—bend in the packaging that forms a divide
wrappers, or accompanying a medical device, related to
between two surfaces of the packaging.
identification, technical description, and use of the medical
device, but excluding shipping documents.
3.1.6 graphic, n—generic schematic of the implant.
3.1.6.1 Discussion—With the schematic, a basic representa- 3.1.11.1 Discussion—Some regional and national regula-
tion of an implant’s features is provided and it may be used to tions refer to “labeling” as “information supplied by the
assist in implant selection by allowing the end user to differ- manufacturer” (ISO 13485, Subclause 3.6 and ISO 15223–1,
entiate it from other systems. Subclause 3.4).
FIG. 1 End of Box
F2943 − 14 (2019)
FIG. 2 Visual Representation of Guide Using ISSL as Primary Identifier on the End of the Box
FIG. 3 Another Visual Representation of Guide Using ISSL as Primary Identifier on the End of the Box
3.1.12 primary label, n—“main” package label of an 4. Significance and Use
implant, which includes all labeling needs such as regulatory
4.1 Implantable medical device labeling often results in a
requirements, an individual manufacturer’s needs, and infor-
variety of label formats and information prioritization. This
mation for implant selection.
variability can be seen not only across different manufacturers
3.1.12.1 Discussion—Information may be included on any
but also across different implant types. At present label design
or all surfaces of an implant’s packaging. Formatting and
andlayoutisdevelopedbyagivenmanufacturerandrepresents
information location of this label is at the discretion of the
balancing internal needs (such as manufacturing, distribution,
manufacturer based on regulatory requirements.
and marketing), regulatory requirements within various
3.1.13 primary size, n—main size designator when selecting
markets, and end user needs (as identified by individual
the implant.
manufacturers performing “voice of the consumer” feedback
on their label designs).
3.1.14 secondary features, n—additional sizes or character-
istics (such as coatings, porous surfaces, groups, offsets,
4.2 At no fault to any given manufacturer, this process,
component capability, and so forth) that aid in appropriate
alongwiththemannerinwhichlabelinformationcompetesfor
selection of the selected implant.
available “real estate” on a package, often leads to variable
prioritization of label information and highly variable label
3.1.15 system, n—brand name or “family” to which the
designs. The impact of this variability on patient care is not
implant belongs.
well documented within the published literature. An article
3.2 Definitions of Terms Specific to This Standard:
3.2.1 musculoskeletal implant, n—for this guide, this termi-
nology shall include all implant types utilized for the care of
Lowry, K. J., McGrath, M. S., Mihalko, W. M., “The Impact of Standardized
musculoskeletal-based conditions, including arthroplasty,
Implant Labels,” AAOS Now, March 2009, (http://www.aaos.org/news/aaosnow/
spine, fracture care, and tissue-engineered products. mar09/clinical12.asp).
F2943 − 14 (2019)
FIG. 4 Additional Example of Guide Using ISSL as Primary Identifier on the End of the Box
from AAOS Now in 2009 described potential issues around (FDA), and the Canadian Healthcare System. The task group
label variability and gave anecdotal evidence of its impact. utilized “voice of consumer” feedback from previous manu-
facturer label initiatives combined with input from various end
4.3 No published literature demonstrating a clear and con-
usersonthetaskgroup.Thisprocessdidnotidentifyanygiven
clusive impact on patient safety resulting from implant label
implant label format as being more or less effective but only
variability was identified. Despite this lack of evidence, anec-
attempts to prioritize information and recommend a universal
dotal observations and input from various involved individuals
formatforthisinformation.Amanufacturermaydeterminethat
and organizations (surgeons, operating room nurses, hospital
an alternative format may be more effective for its internal
administrators, product representatives, and manufacturers)
processes and elect not to follow these recommendations.
suggests a potential, although unproven, benefit for an in-
creased standardization of implant labeling.
5. General Considerations
4.4 The authors of this guide believe it is important to
5.1 Labeling needs are often driven by competing regula-
highlight that no universally accepted method for validation of
tory requirements, manufacturing/distribution needs, and final
a label’s effectiveness exists. Current validation methods con-
implant selection needs.
sist of varying methods of customer feedback on an existing
5.2 The goal of this guide is achieved by creating an ISSL
label design using formal customer questionnaires, informal
area of an implant’s primary label which uniformly (across
customer feedback through individual polling, and internal
differingimplantsandmanufacturers)presentsinformationina
manufacturer-driven studies. The label recommendations pre-
consistently organized format, in an easy-to-view and unclut-
sentedwithinthisguidehavenotbeenvalidatedasmoreorless
tered manner (see examples in Figs. 2-4).
effective than other existing implant labels currently in use.
4.5 These recommendations have been developed through
TABLE 1 Suggested Color Contrasts
the collaboration of an ASTM-sponsored task group with
Text Background
representation from large and small orthopedic implant
Black White
manufacturers, orthopedic surgeons (specifically the Biomedi-
White Blue
cal Engineering Committee from the American Academy of
Blue White
White Black
Orthopedic Surgeons), healthcare facility administrators, oper-
ating room nurses, the U.S. Food and Drug Administration
F2943 − 14 (2019)
5.3 The ISSLwas developed to satisfy the needs of implant 6. ISSL Location
selection as well as a manufacturer’s distribution and packag-
6.1 The preferred or primary location of the ISSLis the end
ing needs.
of the box for a given implant.
5.3.1 The following general considerations are to be applied
to the ISSLand a manufacturer is encouraged to consider them 6.2 The alternate or secondary location of the ISSLis below
the fold of the end of the box, on the adjacent surface.
when developing additional areas of an implant’s label. Addi-
tional information and recommendations may be found in the
6.3 Selection between the preferred or alternate location of
article by Haene.
the ISSL is at the discretion of the manufacturer based on
5.3.2 Universally accepted and published validation meth-
package size restrictions or a manufacturer’s internal needs.
ods of package labeling for orthopedic implants do not
6.3.1 It is recognized that placement of the ISSL below the
currently exist. Therefore, manufacturers are encouraged to
fold of the e
...






Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.