ASTM F1828-97(2006)
(Specification)Standard Specification for Ureteral Stents
Standard Specification for Ureteral Stents
ABSTRACT
This specification covers the chemical, mechanical, and metallurgical requirements for wrought titanium-12 molybdenum- 6 zirconium-2 iron alloy for surgical implants to be used in the manufacture of surgical implants. The heat analysis shall conform to the chemical composition requirements prescribed. Ingot analysis may be used for reporting all chemical requirements, except hydrogen. The wrought titanium-12 molybdenum-6 zirconium-2 iron alloy are classified as bar, forging bar and wire. The ultimate tensile strength, yield strength, elongation, and area reduction of the material shall be tested to meet the requirements prescribed.This specification covers the referee test methods for evaluating the performance characteristics of a single-use ureteral stent with retaining means at both ends, during short term use for drainage of urine from the kidney to the bladder. Ureteral stents shall be tested in accordance with the appropriate biological tests to meet the requirements prescribed. Retention strength, break strength, elongation, dynamic frictional force, and radiopacity shall be tested to meet the requirements prescribed.
SCOPE
1.1 This specification covers the referee test methods for evaluating the performance characteristics of a single-use ureteral stent with retaining means at both ends, during short term use for drainage of urine from the kidney to the bladder. These stents are typically available in diameters of 3.7 Fr to 14.0 Fr, and lengths of 8 cm to 30 cm, and are made of silicone, polyurethane, and other polymers. They are provided non-sterile for sterilization and sterile for single-use.
1.2 Exclusions—Long-term indwelling usage (over 30 days) is encountered with this product, but not commonly, and is therefore considered an exception to this specification. Similarly, the use of ureteral stents for non-ureteral applications such as nephrostomy and ileostomy is excluded from the scope of this specification. Non-sterile ureteral stents are also excluded due to the variability of hospital sterilization equipment and processes and the resulting effects on ureteral stent characteristics.
1.3 The following precautionary statement pertains only to the test method portion, Section 5, of this specification:
1.4 This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety and health practices and determine the applicability of regulatory limitations prior to use.
General Information
Relations
Standards Content (Sample)
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Contact ASTM International (www.astm.org) for the latest information
Designation:F1828 −97(Reapproved 2006)
Standard Specification for
Ureteral Stents
This standard is issued under the fixed designation F1828; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (´) indicates an editorial change since the last revision or reapproval.
INTRODUCTION
The objective of this specification is to describe the test methods used to evaluate the safety and
effectiveness of an indwelling ureteral stent, having retention means at the kidney and bladder ends,
used for urinary drainage of the kidney to the bladder via the ureter.
This specification includes referee test methods that can be used to evaluate the performance
characteristics of ureteral stents. Note that the test methods are not to be construed as production
methods, quality control techniques, or manufacturer’s lot release criteria. The product parameters
addressed by the standard include those determined by the ASTM task group to be pertinent to the
product.
1. Scope 2. Referenced Documents
1.1 This specification covers the referee test methods for 2.1 ASTM Standards:
evaluating the performance characteristics of a single-use D412 Test Methods forVulcanized Rubber andThermoplas-
ureteral stent with retaining means at both ends, during short tic Elastomers—Tension
term use for drainage of urine from the kidney to the bladder. F640 Test Methods for Determining Radiopacity for Medi-
These stents are typically available in diameters of 3.7 Fr to cal Use
14.0Fr,andlengthsof8cmto30cm,andaremadeofsilicone, F748 PracticeforSelectingGenericBiologicalTestMethods
polyurethane, and other polymers. They are provided non- for Materials and Devices
sterile for sterilization and sterile for single-use.
3. Terminology
1.2 Exclusions—Long-termindwellingusage(over30days)
3.1 Definitions of Terms Specific to This Standard:
is encountered with this product, but not commonly, and is
3.1.1 artificial urine—a solution of organic and inorganic
therefore considered an exception to this specification.
compounds that closely simulates the chemical and physical
Similarly, the use of ureteral stents for non-ureteral applica-
properties of normal human urine.Artificial urine will be used
tions such as nephrostomy and ileostomy is excluded from the
asasubstituteforhumanurinetosimulatetheeffectsofhuman
scope of this specification. Non-sterile ureteral stents are also
urine on ureteral stents.
excluded due to the variability of hospital sterilization equip-
ment and processes and the resulting effects on ureteral stent 3.1.2 bladder retention means—physical feature of bladder
end of stent the prevents movement of stent out of bladder.
characteristics.
3.1.3 break strength—peak tensile load required to break
1.3 The following precautionary statement pertains only to
stent.
the test method portion, Section 5, of this specification:
3.1.4 cross section—view of stent tube when cut in a plane
1.4 This standard does not purport to address all of the
perpendicular to length of stent.
safety concerns, if any, associated with its use. It is the
responsibility of the user of this standard to establish appro-
3.1.5 distal—situated away from the point of origin. The
priate safety and health practices and determine the applica-
distal end of a stent is the end that resides in the bladder, also
bility of regulatory limitations prior to use.
known as the bladder end.
3.1.6 drainage holes—holes in wall of stent tubing that
allow flow of urine into and out of lumen of stent.
This specification is under the jurisdiction of ASTM Committee F04 on
Medical and Surgical Materials and Devices and is the direct responsibility of
Subcommittee F04.34 on Urological Materials and Devices. For referenced ASTM standards, visit the ASTM website, www.astm.org, or
Current edition approved March 1, 2006. Published April 2006. Originally contact ASTM Customer Service at service@astm.org. For Annual Book of ASTM
approved in 1997. Last previous edition approved in 1997 as F1828 – 97. DOI: Standards volume information, refer to the standard’s Document Summary page on
10.1520/F1828-97R06. the ASTM website.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959. United States
F1828−97 (2006)
3.1.7 dynamic frictional force—resistancetorelativemotion The manufacturer need not use this referee test method for
between two surfaces during motion. This force is defined as inspection and quality control.
the coefficient of kinetic friction multiplied by the force acting
3.1.16 retention strength—force required to overcome the
on the surface of the material in a plane perpendicular to the
retaining means on a stent.
surface.
3.1.17 sterility—the state of being free of microorganisms.
3.1.8 elongation—expressed as a percent, is equal to the
For purposes of this specification, sterility is defined as
change in length of a sample of tubing at failure divided by its
freedom from microorganisms when tested according to the
original length. Stretching of the tubing is produced by tensile
methodology defined by the USP for nonparenteral devices.
loading.
3.1.18 tolerances—the allowable deviation from a standard
3.1.9 French size—Scale used to indicate size of tubular
size. The tolerance for the length of a ureteral stent is 60.5 cm
devices, each unit being approximately equal to 0.013 in. or
(0.197 in). the tolerance for the specified French size of a
0.33 mm in diameter.Typical label French sizes are as follows:
ureteral stent is 60.01 mm (0.004 in), or approximately ⁄3
French Size Outside Diameter
French.
in. mm
3.1.19 ureteral stent—an indwelling tubular device that
3.7 0.050,1.23
resides in the kidney, ureter, and bladder containing means for
4.5 0.060,1.50
retaining ends of tube in kidney and bladder.
4.7 0.061,1.57
6.0 0.079,2.00
7.0 0.092,2.33
4. Requirements
8.0 0.105,2.67
8.5 0.112,2.83
4.1 Biocompatibility—Ureteral stents shall be tested in ac-
10.0 0.131,3.33
cordance with the appropriate biological tests contained in
14.0 0.183,4.66
Specification F748 or similar guidance established by the U. S.
3.1.10 kidney retention means—physical feature of kidney
Food and Drug Administration or International Organization
end of stent that prevents movement of stent out of the kidney.
for Standardization (ISO).
3.1.11 length—length of stent is defined as the distance
between the most proximal portion of the bladder retention
5. Special Precautions
means and the most distal portion of the kidney retention
5.1 The following cautionary comments recognize the sen-
means when the stent is laying on a flat surface with the
sitivity of the materials of construction to potential environ-
mainshaft straight. (See Fig. 1).
mental conditions. These are outlined here to point out poten-
3.1.12 lumen—the channel within a tube.
tialsituationsthatcouldadverselyaffecttheperformanceofthe
3.1.13 proximal—situated toward the point of origin. In the
stent during testing.
urinary tract, the kidney is considered to be the point of origin.
5.1.1 Care should be taken during testing and use to prevent
The proximal end of a stent is the end that resides in the renal
damage to the stents. Such damage can be caused by abrasion
pelvis, also known as the kidney end.
and contact with sharp objects or chemical products.
3.1.14 radiopacity—property indicating ability of device to
5.1.2 Stents should be kept away from generators, electric
absorbx-rayenergy,allowingdevicetobeseeninaradiograph
motors,diathermymachines,andfluorescentlightsbecausethe
or fluoroscopic screen.
ozone produced may attack elastomeric materials. This applies
to both storage and handling.
3.1.15 referee test method—the method cited in the pub-
lished specification for the device. This method will be used 5.1.3 To help avoid contamination of the stents proper
when the performance of the ureteral stent is to be evaluated. handling precautions should be observed.
FIG. 1Determine of Stent Length
F1828−97 (2006)
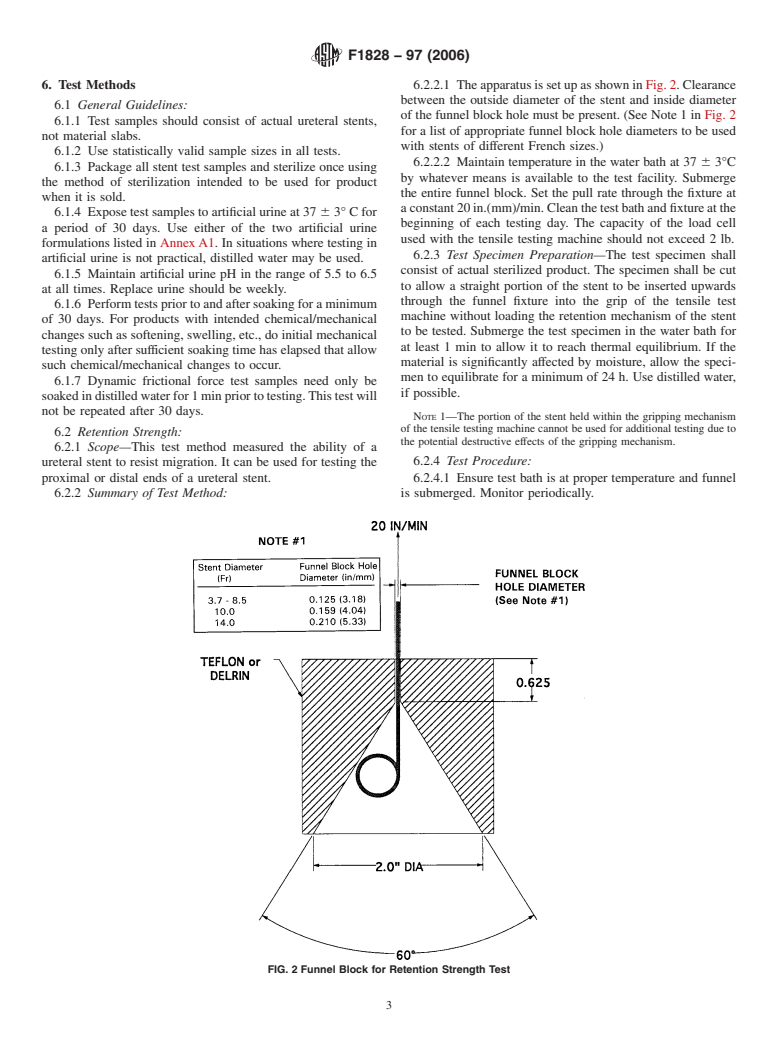
6. Test Methods 6.2.2.1 TheapparatusissetupasshowninFig.2.Clearance
between the outside diameter of the stent and inside diameter
6.1 General Guidelines:
of the funnel block hole must be present. (See Note 1 in Fig. 2
6.1.1 Test samples should consist of actual ureteral stents,
for a list of appropriate funnel block hole diameters to be used
not material slabs.
with stents of different French sizes.)
6.1.2 Use statistically valid sample sizes in all tests.
6.2.2.2 Maintain temperature in the water bath at 37 6 3°C
6.1.3 Package all stent test samples and sterilize once using
by whatever means is available to the test facility. Submerge
the method of sterilization intended to be used for product
the entire funnel block. Set the pull rate through the fixture at
when it is sold.
aconstant20in.(mm)/min.Cleanthetestbathandfixtureatthe
6.1.4 Expose test samples to artificial urine at 37 6 3° C for
beginning of each testing day. The capacity of the load cell
a period of 30 days. Use either of the two artificial urine
used with the tensile testing machine should not exceed 2 lb.
formulations listed in AnnexA1. In situations where testing in
6.2.3 Test Specimen Preparation—The test specimen shall
artificial urine is not practical, distilled water may be used.
consist of actual sterilized product. The specimen shall be cut
6.1.5 Maintain artificial urine pH in the range of 5.5 to 6.5
to allow a straight portion of the stent to be inserted upwards
at all times. Replace urine should be weekly.
through the funnel fixture into the grip of the tensile test
6.1.6 Performtestspriortoandaftersoakingforaminimum
machine without loading the retention mechanism of the stent
of 30 days. For products with intended chemical/mechanical
to be tested. Submerge the test specimen in the water bath for
changes such as softening, swelling, etc., do initial mechanical
at least 1 min to allow it to reach thermal equilibrium. If the
testing only after sufficient soaking time has elapsed that allow
material is significantly affected by moisture, allow the speci-
such chemical/mechanical changes to occur.
men to equilibrate for a minimum of 24 h. Use distilled water,
6.1.7 Dynamic frictional force test samples need only be
if possible.
soakedindistilledwaterfor1minpriortotesting.Thistestwill
not be repeated after 30 days.
NOTE 1—The portion of the stent held within the gripping mechanism
of the tensile testing machine cannot be used for additional testing due to
6.2 Retention Strength:
the potential destructive effects of the gripping mechanism.
6.2.1 Scope—This test method measured the ability of a
6.2.4 Test Procedure:
ureteral stent to resist migration. It can be used for testing the
proximal or distal ends of a ureteral stent. 6.2.4.1 Ensure test bath is at proper temperature and funnel
6.2.2 S
...







Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.