ASTM F981-99(2003)
(Practice)Standard Practice for Assessment of Compatibility of Biomaterials for Surgical Implants with Respect to Effect of Materials on Muscle and Bone
Standard Practice for Assessment of Compatibility of Biomaterials for Surgical Implants with Respect to Effect of Materials on Muscle and Bone
SCOPE
1.1 This practice provides a series of experimental protocols for biological assays of tissue reaction to nonabsorbable biomaterials for surgical implants. It assesses the effects of the material on animal tissue in which it is implanted. The experimental protocol is not designed to provide a comprehensive assessment of the systemic toxicity, immune response, carcinogenicity, teratogenicity, or mutagenicity of the material since other standards deal with these issues. It applies only to materials with projected applications in humans where the materials will reside in bone or soft tissue in excess of 30 days and will remain unabsorbed. It is recommended that short-term assays, according to Practice F 763, first be performed. Applications in other organ systems or tissues may be inappropriate and are therefore excluded. Control materials will consist of any one of the metal alloys in Specifications F 67, F 75, F 90, F 136, F 138, or F 562, high purity dense aluminum oxide as described in Specification F 603, ultra high molecular weight polyethylene as stated in Specification F 648 or USP polyethylene negative control.
1.2 This practice is a combination of Practice F 361 - 80 and Practice F 469 - 78. The purpose, basic procedure, and method of evaluation of each type of material are similar; therefore, they have been combined.
This standard does not purport to address all of the safety concerns, if any, associated with its use. It is the responsibility of the user of this standard to establish appropriate safety and health practices and determine the applicability of regulatory limitations prior to use.
General Information
Relations
Standards Content (Sample)
NOTICE: This standard has either been superseded and replaced by a new version or withdrawn.
Contact ASTM International (www.astm.org) for the latest information
Designation: F 981 – 99 (Reapproved 2003)
Standard Practice for
Assessment of Compatibility of Biomaterials for Surgical
Implants with Respect to Effect of Materials on Muscle and
Bone
This standard is issued under the fixed designation F 981; the number immediately following the designation indicates the year of
original adoption or, in the case of revision, the year of last revision. A number in parentheses indicates the year of last reapproval. A
superscript epsilon (e) indicates an editorial change since the last revision or reapproval.
1. Scope Implant Applications (UNS R50250, UNS R50400, UNS
R50550, UNS R50700)
1.1 This practice provides a series of experimental protocols
F 75 Specification for Cobalt-28Chromium-6Molybdenum
for biological assays of tissue reaction to nonabsorbable
Alloy Castings and Casting Alloy for Surgical Implants
biomaterials for surgical implants. It assesses the effects of the
(UNS R30075)
material on animal tissue in which it is implanted. The
F 86 Practice for Surface Preparation and Marking of Me-
experimental protocol is not designed to provide a comprehen-
tallic Surgical Implants
sive assessment of the systemic toxicity, immune response,
F 90 Specification for Wrought Cobalt20-Chromium15-
carcinogenicity, teratogenicity, or mutagenicity of the material
Tungsten10-Nickel Alloy for Surgical Implant Applica-
since other standards deal with these issues. It applies only to
tions (UNS R30605)
materials with projected applications in humans where the
F 136 Specification for Wrought Titanium-6Aluminum-
materials will reside in bone or soft tissue in excess of 30 days
4Vanadium ELI (Extra Low Interstitial) Alloy for Surgical
and will remain unabsorbed. It is recommended that short-term
Implant Applications (UNS R56401)
assays, according to Practice F 763, first be performed. Appli-
F 138 Specification for Wrought-18Chromium-14Nickel-
cations in other organ systems or tissues may be inappropriate
2.5Molybdenum Stainless Steel Bar and Wire for Surgical
and are therefore excluded. Control materials will consist of
Implants (UNS S31673)
any one of the metal alloys in Specifications F 67, F 75, F 90,
F 361 Practice for Assessment of Compatibility of Metallic
F 136, F 138, or F 562, high purity dense aluminum oxide as
Materials for Surgical Implants with Respect to Effect of
described in Specification F 603, ultra high molecular weight
Materials on Tissue
polyethylene as stated in Specification F 648 or USP polyeth-
F 469 Practice for Assessment of Compatibility of Nonpo-
ylene negative control.
rous Polymeric Materials for Surgical Implants with Re-
1.2 This practice is a combination of Practice F 361 – 80
gard to Effect of Materials on Tissue
and Practice F 469 – 78. The purpose, basic procedure, and
F 562 Specification for Wrought Cobalt-35Nickel-
method of evaluation of each type of material are similar;
20Chromium-10Molybdenum Alloy for Surgical Implant
therefore, they have been combined.
Applications (UNS R30035)
1.3 This standard does not purport to address all of the
F 603 Specification for High-Purity Dense Aluminum Ox-
safety concerns, if any, associated with its use. It is the
ide for Surgical Implant Application
responsibility of the user of this standard to establish appro-
F 648 Specification for Ultra-High-Molecular-Weight Poly-
priate safety and health practices and determine the applica-
ethylene Powder and Fabricated Form for Surgical Im-
bility of regulatory limitations prior to use.
plants
2. Referenced Documents F 763 Practice for Short-Term Screening of Implant Mate-
rials
2.1 ASTM Standards:
F 67 Specification for Unalloyed Titanium for Surgical
3. Summary of Practice
3.1 This practice describes the preparation of implants, the
number of implants and test hosts, test sites, exposure sched-
This practice is under the jurisdiction of ASTM Committee F04 on Medical and
Surgical Materials and Devices and is the direct responsibility of Subcommittee
ule, implant sterilization techniques, and methods of implant
F04.16 on Biocompatibility Test Methods.
retrieval and tissue examination of each test site. Histological
Current edition approved Nov. 1, 2003. Published December 2003. Originally
criteria for evaluating tissue reaction are provided.
approved in 1986. Last previous edition approved in 1999 as F 981 – 99.
For referenced ASTM standards, visit the ASTM website, www.astm.org, or
contact ASTM Customer Service at service@astm.org. For Annual Book of ASTM
Standards volume information, refer to the standard’s Document Summary page on
the ASTM website. Withdrawn.
Copyright © ASTM International, 100 Barr Harbor Drive, PO Box C700, West Conshohocken, PA 19428-2959, United States.
F 981 – 99 (2003)
4. Significance and Use 6.3.1 The implants shall be cylindrical in shape and may
range from 1 mm to 6 mm in diameter and from 10 mm to 20
4.1 This practice covers a test protocol for comparing the
mm in length depending upon the relative size of the species
local tissue response evoked by biomaterials, from which
under study.
medical implantable devices might ultimately be fabricated,
6.3.2 The dimensions used shall be reported in accordance
with the local tissue response elicited by control materials
with 8.1.
currently accepted for the fabrication of surgical devices. The
6.3.3 Depending upon the particular device application,
materials may include metals (and metal alloys), dense alumi-
other sample shapes may be used. For instance, an investigator
num oxide, and polyethylene that are standardized on the basis
might wish to test the biocompatibility of a new material for
of acceptable long-term well-characterized long-term response.
screws in the form of a screw. If an alternative specimen shape
The controls consistently produce cellular reaction and wound
is used, this should be reported in accordance with 8.1.
healing to a degree that has been found to be acceptable to the
6.4 Sizes and Shapes of Implants for Insertion in Bone:
host.
6.4.1 Implant diameters for use in bone shall be approxi-
mately equal to the cortex thickness. Implant lengths shall
5. Test Hosts and Sites
allow them to reside in one cortex and the medulla without
5.1 Rats (acceptable strains such as Fischer 344), New
excessive protrusion beyond the periosteum.
Zealand White rabbits, and other small laboratory animals may
6.4.2 The dimensions used shall be reported in accordance
be used as test hosts for soft tissue implant response. It is
with 8.1.
suggested that the rats be age and sex matched. Rabbits or
6.5 Number of Test and Control Implants:
larger animals may be used as test hosts for bone implants.
6.5.1 In each rat, due to size, there may be two implants; one
When larger animals such as dogs, goats, or sheep are used, the
each test and control material implant.
decision should be based upon special considerations of the
6.5.2 In each rabbit, due to size, there may be six implants;
particular implant material or study.
four test materials and two control material implants.
5.2 The sacro-spinalis, paralumbar, gluteal muscles, and the
6.5.3 In larger animals, there may be twelve implants; eight
femur or tibia can serve as the test site for implants. However,
test materials and four control material implants.
the same site must be used for test and material implants in all
6.5.4 In rabbits or larger animals, there shall be tested at
the animal species.
least sixteen test material implants and eight control material
5.3 There shall be a minimum of four animals at each
implants at each time period.
sacrifice interval for a total of twelve animals per study. If
6.6 Conditioning:
larger animals are used, in which a greater number of implants
6.6.1 Remove all surface contaminants with appropriate
can be placed, there shall be at least two animals sacrificed at
solvents and rinse all test and control implants in distilled water
each time period.
prior to sterilization. It is recommended that the implant
materials be processed and cleaned in the same way the final
6. Implant Specimens
product will be.
6.1 Fabrication— Each implant shall be made in a cylin-
6.6.2 Clean, package, and sterilize all implants in the same
drical shape with hemispherical ends (see 6.3 and 6.4 for
way as used for human implantation.
sizes). If the ends are not hemispherical, this shall be reported.
6.6.3 After final preparation and sterilization, handle the test
Each implant shall be fabricated, finished, and its surface
and control implants with great care to ensure that they are not
cleaned in a manner appropriate for its projected application in
scratched, damaged, or contaminated in any way prior to
human subjects in accordance with Practice F 86. If the
insertion.
specimens are porous, the method of preparation of the porous
6.6.4 Report all details of conditioning in accordance with
specimens shall be representative of the contemplated human
8.1.
implant application and shall yield a specimen with character-
6.7 Implantation Period—Insert all implants into each ani-
istic pore size, pore volume, and pore interconnection diameter.
mal at the same surgical session for implantation periods of 12,
The choice between using solid core specimens with porous
26, and 52 weeks.
coatings and specimens that are porous throughout shall be a
decision of the investigator and shall be reported.
7. Procedure
6.2 Reference metallic specimens shall be fabricated in
7.1 Implantation (Muscle):
accordance with 6.1 from materials such as the metal alloys in
Specifications F 67, F 75, F 90, F 138, or F 562, ceramic in
7.1.1 Place material implants in the paravertebral muscles in
Specification F 603, or polymers such as in Specification F 648
such a manner that they are directly in contact with muscle
polyethylene or USP Negative Control Plastic. If the test
tissue.
materials are porous, consideration should be given to using
7.1.2 Introduce material implants in larger animals by the
porous specimens for reference specimens. Alternatively, non-
technique of making an implantation site in the muscle by
porous reference specimens may be used.
using a hemostat to separate the muscle fibers. Then insert the
6.3 Suggested Sizes and Shapes of Implants for Insertion in implant using plastic-tipped forceps or any tool that is non-
Muscle: abrasive to avoid damage to the implant.
F 981 – 99 (2003)
7.1.3 Introduce material implants using sterile technique. 7.6.1 Tissue Sample Preparation—Prepare appropriate
Sterile disposable needles or hypodermic tubing and trochar blocks from each implantation site and indicate the orientation
may be used to implant the material implants into the paraver- of the axis of the femur relative to the axis of the implant (for
tebral muscles along the spine. In rats, insert a negative control bone implants). Also indicate the orientation of the implant
implant on one side of the spine and a test material implant on relative to the axis of rotation of the femoral condyles.
the other side. In rabbits, implant one negative control material 7.6.1.1 Process the excised tissue block containing either a
on each side of the spine and implant two test materials on each test implant or control implant for histopathological examina-
side of the spine. If larger diameter specimens are used, an tion and such other studies as are appropriate. Cut the sample
alternative implantation technique is that described in 7.1.2. midway from end to end into appropriate size and in the
7.2 Implantation (Femur)—Expose the lateral cortex of appropriate orientation for each study. Transfer, or record, or
both, the orientational details noted in 7.6.1 to each part of the
each rabbit femur and drill undersized pilot holes through the
lateral cortex using the technique and instrument appropriate sample. Record the gross appearance of the implant and the
tissue. If the sample is porous, it is imperative that sectioning
for the procedure. Final reaming of the holes should be
performed by hand to yield holes which are smaller than the procedures be used that maintain the implant within its tissue
envelope to allow the evaluation of tissue within the pores.
implant specimens by 0.1 mm or less. Into each one of these
Such procedures may include ground section preparation.
holes, insert one of the implants by finger pressure. Then close
7.6.1.2 If special stains are deemed necessary, prepare
the wound.
additional sections and make appropriate observations.
NOTE 1—Caution should be taken to minimize the motion of the
7.7 Histopathological Observations—Compare the amount
implant in the tissue to prevent the effects of motion on the desired result.
of tissue reaction adjacent to the test implant to that adjacent to
7.3 Postoperative Care:
a similar location and orientation on the control implant with
7.3.1 All animal studies must be done in a facility approved respect to thickness of scar, presence of inflammatory or other
by a nationally recognized organization and in accordance with cell types, presence of particles, and such other indications of
all appropriate regulations. interaction of tissue and material as might occur with the actual
7.3.2 Carefully observe each animal during the period of material under test. A suggested method for the evaluation of
tissue response after implantation is Turner, et al. (1) .Ifa
assay and report any abnormal findings.
porous sample is being tested, the evaluation of the tissue
7.3.3 Infection or injury of the test implant site may
reaction must include areas within the pores of the test and
invalidate the results. The decision to replace the animal so that
control samples at similar locations.
the total number of retrieved implants will be as represented in
7.7.1 Suggested Method for Tissue Response Evaluation:
the schedule shall be dependent upon the design of the study.
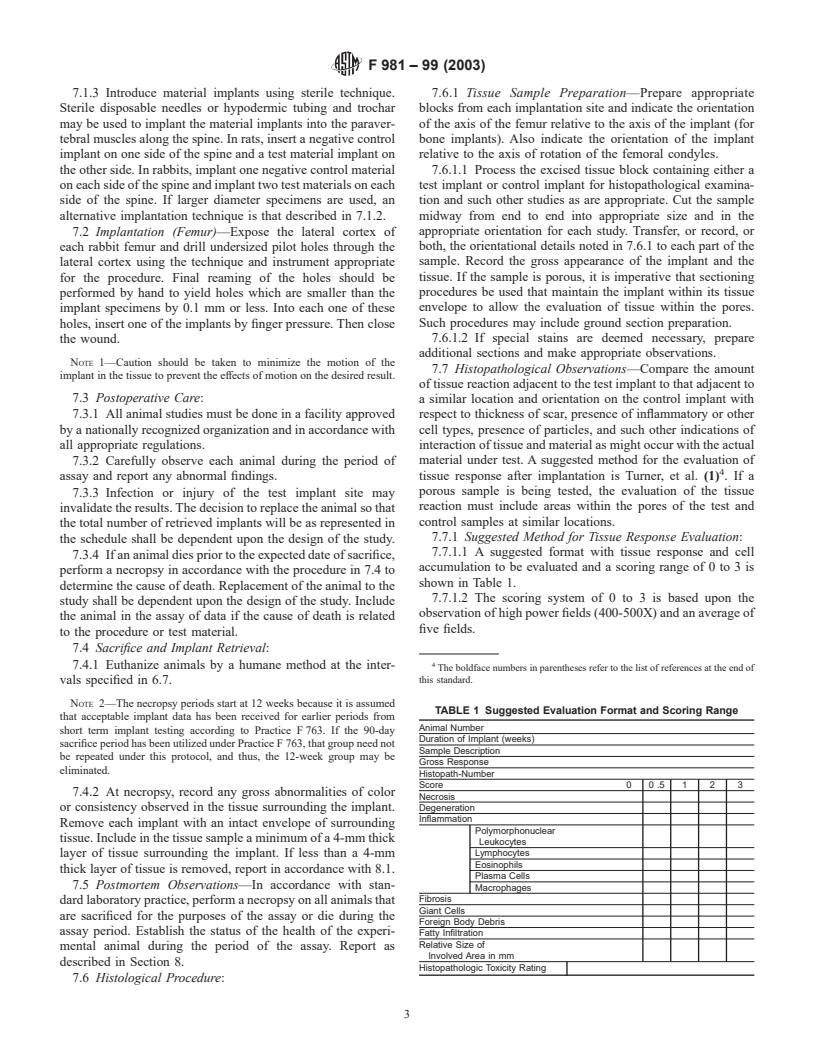
7.7.1.1 A suggested format with tissue response and cell
7.3.4 If an animal dies prior to the expected date of sacrifice,
accumulation to be evaluated and a scoring range of 0 to 3 is
perform a necropsy in accordance with the procedure in 7.4 to
shown in Table 1.
determine the cause of death. Replacement of the animal to the
7.7.1.2 The scoring system of 0 to 3 is based upon the
study shall be dependent upon the design of the study. Include
observation of high power fields (400-500X) and an average of
the animal in the assay of data if the cause of death is related
five fields.
to the procedure or test material.
7.4 Sacrifice and Implant Retrieval:
7.4.1 Euthanize animals by a humane method at the inter-
The boldface numbers in parentheses refer to the list of references at the end of
vals specified in 6.7. this standard.
NOTE 2—The necropsy periods start at 12 weeks because it is assumed
TABLE 1 Suggested
...







Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.