ISO 45006:2023
(Main)Occupational health and safety management — Guidelines for organizations on preventing, controlling and managing infectious diseases
Occupational health and safety management — Guidelines for organizations on preventing, controlling and managing infectious diseases
This document gives guidelines for organizations on how to prevent or control exposure to infectious agents at the workplace and manage the risks associated with infectious diseases that: — present a risk of severe ill health or death and can impact the health, safety and well-being of workers and other relevant interested parties; — present a lower risk to health yet have a significant impact on the organization, its workers and other relevant interested parties. This document is applicable to organizations of all sizes and sectors. NOTE This document does not provide comprehensive guidance to those parts of an organization that implement mandated infection controls such as hospitals and medical or biological laboratories because there is an inherent potential for exposure to infectious diseases. Applicable legislation and guidance are provided by government, regulators and health authorities for specific infection controls for the protection of workers in such settings and for work activities on or with pathogenic microorganisms.
Management de la santé et de la sécurité au travail — Lignes directrices sur la prévention, le contrôle et la prise en charge des maladies infectieuses destinées aux organismes
Sistem vodenja varnosti in zdravja pri delu - Smernice organizacijam za preprečevanje in obvladovanje nalezljivih bolezni
Ta dokument podaja smernice za organizacije, kako preprečiti izpostavljenost nalezljivim boleznim in obvladovati tveganja povezanih z njimi, ki: – predstavljajo tveganje hude bolezni ali smrti in lahko vplivajo na zdravje, varnost in dobro počutje delavcev in zadevnih zainteresiranih strani; – predstavljajo manjše tveganje za zdravje, vendar pa imajo pomemben vpliv na organizacijo, njene delavce in zadevne zainteresirane strani. Ta dokument se uporablja za organizacije vseh velikosti in z vseh sektorjev. Opomba: Vladni organi, regulatorji in zdravstveni organi določajo veljavno zakonodajo za obvladovanje posebnih nalezljivih bolezni za zaščito delavcev v kliničnem okolju in drugih zdravstvenih ustanovah in za dejavnosti dela s patogenimi mikroorganizmi.
General Information
Relations
Standards Content (Sample)
SLOVENSKI STANDARD
01-februar-2024
Sistem vodenja varnosti in zdravja pri delu - Smernice organizacijam za
preprečevanje in obvladovanje nalezljivih bolezni
Occupational health and safety management - Guidelines for organizations on
preventing and managing infectious diseases
Management de la santé et de la sécurité au travail — Lignes directrices sur la
prévention et la prise en charge des maladies infectieuses destinées aux organismes
Ta slovenski standard je istoveten z: ISO 45006:2023
ICS:
13.100 Varnost pri delu. Industrijska Occupational safety.
higiena Industrial hygiene
2003-01.Slovenski inštitut za standardizacijo. Razmnoževanje celote ali delov tega standarda ni dovoljeno.
INTERNATIONAL ISO
STANDARD 45006
First edition
2023-12
Occupational health and safety
management — Guidelines for
organizations on preventing,
controlling and managing infectious
diseases
Management de la santé et de la sécurité au travail — Lignes
directrices sur la prévention, le contrôle et la prise en charge des
maladies infectieuses destinées aux organismes
Reference number
© ISO 2023
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on
the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address below
or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii
Contents Page
Foreword .v
Introduction . vi
1 Scope . 1
2 Normative references . 1
3 Terms and definitions . 1
4 Context of the organization .4
4.1 General . 4
4.2 External issues . 4
4.3 Internal issues . 5
4.3.1 General . 5
4.3.2 Diversity of workers and other relevant interested parties . 5
5 Characteristics of infectious diseases . 6
6 L eadership and worker participation . 7
6.1 Leadership . 7
6.2 Consultation and participation of workers . 7
6.3 Roles, responsibilities and competence . 8
7 Communication .8
7.1 General . 8
7.2 Methods of communication . 9
7.3 Communication with and reporting to external interested parties. 9
8 Hazards, risks and controls .9
8.1 Identification of hazards . 9
8.2 A ssessment of risks . 10
8.3 Determination of controls . 11
8.3.1 Selection of controls . 11
8.3.2 Hierarchy of controls . 11
8.3.3 Additional considerations for controls .12
8.4 P lanning of changes to controls .12
9 Psychological health and well-being .13
9.1 Psychosocial hazards and risks . 13
9.2 Controls to manage psychosocial risks . 13
10 Resources .14
11 Implementation of controls for infectious diseases .15
11.1 General . 15
11.2 Personal hygiene . 15
11.3 Work-related travel . 16
12 Implementation of controls for contagious diseases .16
12.1 General . 16
12.2 Workplaces under the control of the organization . 17
12.2.1 General workplace infection controls . 17
12.2.2 Use of common areas . 18
12.2.3 Meetings and visits to workplaces . 19
12.2.4 Deliveries . 19
12.3 Working from home . 20
12.4 Working in other people’s homes . 20
12.5 Working in multiple locations . 21
12.6 Working with the public . 22
13 Implementation of controls for non-contagious infectious diseases .22
iii
14 Implementation of controls for endemic diseases .23
15 Use of personal protective equipment and face coverings .23
15.1 General .23
15.2 Selection of appropriate protection . 24
15.2.1 General . 24
15.2.2 Protective gloves . 24
15.2.3 Face and respiratory protection . 25
16 Emergency preparedness and response .26
17 Management of suspected or confirmed cases of a relevant infectious disease .27
17.1 General . 27
17.2 Managing illness in a workplace . 27
17.2.1 General . 27
17.2.2 Occurrence of contagious disease.28
17.3 Screening, testing, contact tracing, quarantine and vaccination .28
18 Per f or m a nc e ev a lu at ion .28
18.1 General .28
18.2 M onitoring and measurement .29
18.3 Analysis and evaluation . 30
18.4 M anagement review . 30
19 Improvement .30
Annex A (informative) Examples of risk tables.32
Bibliography .34
iv
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out
through ISO technical committees. Each member body interested in a subject for which a technical
committee has been established has the right to be represented on that committee. International
organizations, governmental and non-governmental, in liaison with ISO, also take part in the work.
ISO collaborates closely with the International Electrotechnical Commission (IEC) on all matters of
electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are
described in the ISO/IEC Directives, Part 1. In particular, the different approval criteria needed for the
different types of ISO document should be noted. This document was drafted in accordance with the
editorial rules of the ISO/IEC Directives, Part 2 (see www.iso.org/directives).
ISO draws attention to the possibility that the implementation of this document may involve the use
of (a) patent(s). ISO takes no position concerning the evidence, validity or applicability of any claimed
patent rights in respect thereof. As of the date of publication of this document, ISO had not received
notice of (a) patent(s) which may be required to implement this document. However, implementers are
cautioned that this may not represent the latest information, which may be obtained from the patent
database available at www.iso.org/patents. ISO shall not be held responsible for identifying any or all
such patent rights.
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation of the voluntary nature of standards, the meaning of ISO specific terms and
expressions related to conformity assessment, as well as information about ISO's adherence to
the World Trade Organization (WTO) principles in the Technical Barriers to Trade (TBT), see
www.iso.org/iso/foreword.html.
This document was prepared by Technical Committee ISO/TC 283, Occupational health and safety
management.
Any feedback or questions on this document should be directed to the user’s national standards body. A
complete listing of these bodies can be found at www.iso.org/members.html.
v
Introduction
Infectious diseases are increasingly recognized as major challenges to health, safety and well-being.
Decisions and activities relating to the prevention and management of infectious diseases affect workers
within the organization and other people who visit a workplace, come into contact with workers or can
be affected by the organization’s activities. This document is a response to the risks that infectious
diseases present to workers and other relevant interested parties (e.g. customers, the public, suppliers,
workers from other organizations, family members and other personal contacts).
There is a broad range of infectious diseases with potential impacts on health, safety and well-being,
which can vary from very mild to very serious depending on the nature of the infectious disease. Key
characteristics of infectious diseases (see Clause 5) are a major factor in the risk posed to workers and
other relevant interested parties.
Some infectious diseases are non-contagious and infect only the individual who contracts the disease
and do not usually transmit from human to human (e.g. legionellosis or malaria), while others are
contagious and have the potential to spread from a single individual to infect others (e.g. influenza,
COVID-19, smallpox, hepatitis, salmonellosis, tuberculosis, Ebola and HIV/AIDS), up to and including a
pandemic spread of the disease.
The impact in terms of severity of infectious diseases can vary from person to person depending on
underlying health conditions (e.g. asthma, diabetes, obesity, strength of immune system) and factors
such as age, sex and socio-economic situation. Impacts can be more severe where one or more such
circumstances exist.
This document provides guidelines to prevent or reduce exposure to, and transmission of, infectious
agents and to manage risks to workers and other relevant interested parties from infectious diseases. It
supports the principle that workers should not be required to work in settings without implementation
of appropriate prevention and controls.
The guidance is generic and applicable to organizations regardless of the nature of business, service
provision, size or complexity. It recognizes that many smaller organizations do not have dedicated
departments or functions such as occupational health and safety (OH&S), facilities management, human
resources or infectious disease specialists. More detailed information for specific functions is available
from professional bodies and a wide range of national and international standards.
Organizations using ISO 45001 can use this document to improve OH&S management by relating the
relevant clauses to the PDCA cycle:
— Plan: plan what needs to be done for the organization to work safely;
— Do: do what the organization has planned to do;
— Check: see how well it is working;
— Act: take actions to improve or change controls that are not effective.
Taking a system's approach facilitates the coordination of resources and efforts and will enable
organizations to better manage the risk from infectious diseases, by ensuring they are included in
existing OH&S processes.
This document is not intended to be a single step-by-step set of recommendations. It provides guidelines
to enable ongoing continual improvement and to ensure the organization responds to incidents of
infectious diseases, including epidemics and pandemics.
This document is designed to complement ISO 45001 by providing guidelines that align with the
requirements of ISO 45001. This document can be used independently, by any organization, to improve
OH&S performance.
vi
INTERNATIONAL STANDARD ISO 45006:2023(E)
Occupational health and safety management — Guidelines
for organizations on preventing, controlling and managing
infectious diseases
1 Scope
This document gives guidelines for organizations on how to prevent or control exposure to infectious
agents at the workplace and manage the risks associated with infectious diseases that:
— present a risk of severe ill health or death and can impact the health, safety and well-being of workers
and other relevant interested parties;
— present a lower risk to health yet have a significant impact on the organization, its workers and
other relevant interested parties.
This document is applicable to organizations of all sizes and sectors.
NOTE This document does not provide comprehensive guidance to those parts of an organization that
implement mandated infection controls such as hospitals and medical or biological laboratories because there
is an inherent potential for exposure to infectious diseases. Applicable legislation and guidance are provided
by government, regulators and health authorities for specific infection controls for the protection of workers in
such settings and for work activities on or with pathogenic microorganisms.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
ISO 45001:2018, Occupational health and safety management systems — Requirements with guidance for
use
3 Terms and definitions
For the purposes of this document, the terms and definitions given in ISO 45001 and the following apply.
ISO and IEC maintain terminology databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https:// www .iso .org/ obp
— IEC Electropedia: available at https:// www .electropedia .org/
3.1
workplace
place where a person needs to be or to go for work purposes
Note 1 to entry: The organization’s responsibilities for the workplace depend on the degree of control over the
workplace.
Note 2 to entry: Workplaces can be inside or outside and include the worker’s own home, other people’s homes,
personal vehicles, vehicles provided by the organization, other organizations’ facilities and public spaces.
[SOURCE: ISO 45001:2018, 3.6, modified — “under the control of the organization” has been deleted
from the definition, “under the OH&S management system” has been deleted from Note 1 to entry and
Note 2 to entry has been added.]
3.2
legal requirements and other requirements
legal requirements that an organization has to comply with and other requirements that an organization
has to or chooses to comply with
[SOURCE: ISO 45001:2018, 3.9, modified — Notes 1, 2 and 3 to entry have been deleted.]
3.3
top management
person or group of people who directs and controls an organization at the highest level
[SOURCE: ISO 45001:2018, 3.12, modified — Notes 1, 2 and 3 to entry have been deleted.]
3.4
incident
occurrence arising out of, or in the course of, work that can or does result in injury and ill health
Note 1 to entry: In this document, “injury and ill health” refers to contracting an infectious disease (3.8) or any
identifiable, adverse physical or psychological condition arising from or associated with an infectious disease.
[SOURCE: ISO 45001:2018, 3.35, modified — Note 1 to entry has been replaced, and Notes 2 and 3 to
entry have been deleted.]
3.5
personal protective equipment
PPE
device or appliance designed to be worn by an individual for their protection against one or more health
and safety hazards
Note 1 to entry: PPE includes, but is not limited to, gowns, gloves, respirators, safety glasses, helmets and goggles.
Note 2 to entry: While generally not considered PPE, masks, and other face coverings (3.6) can provide a level of
protection for the user in addition to their primary purpose as a public health measure to control the spread of
transmission and infection.
Note 3 to entry: In many countries, PPE is required to conform to national regulations.
[SOURCE: ISO 15384:2018, 3.12, modified — “or held” have been deleted after “worn” and “their” has
been added before “protection” in the definition, and Notes 1, 2 and 3 to entry have been added.]
3.6
face covering
facepiece that covers the mouth, nose and chin
EXAMPLE ‘community masks’, ‘hygiene masks’, ‘barrier masks’, and ‘comfort masks’ are all examples of face
coverings.
Note 1 to entry: Face coverings in the context of this document are not considered to be personal protective
equipment (PPE) (3.5) or a medical device.
3.7
well-being
fulfilment of the physical, mental and cognitive needs and expectations of a worker related to their
work
Note 1 to entry: Well-being can also contribute to the quality of life outside of work.
Note 2 to entry: Well-being relates to all aspects of working life, including work organization, social factors at
work, work environment, equipment and hazardous tasks.
[SOURCE: ISO 45003:2021, 3.2, modified — “at work” has been deleted after “well-being” from the term
and Notes 1 and 2 to entry have been added.]
3.8
common area
space and amenity provided for the use of more than one person
EXAMPLE Canteens, lifts/elevators, stairs, reception areas, meeting rooms, areas of worship, toilets,
gardens, fire escapes, kitchens, fitness facilities, store rooms, laundry facilities.
Note 1 to entry: Common areas can include spaces and amenities used by more than one organization.
Note 2 to entry: Common areas can include spaces and amenities where people are working.
[SOURCE: ISO/PAS 45005:2020, 3.11, modified — the term "common areas" has been changed to
"common area", "spaces and amenities" has been changed to "space and amenity" in the definition, and
Notes 1 and 2 to entry have been added.]
3.9
infectious disease
condition caused by agents such as bacteria, viruses, prion, parasites or fungi that can spread, directly
or indirectly, and that can result in ill-health
Note 1 to entry: In this document, “infectious disease” refers to a disease that:
— presents a risk of severe ill health or death and can impact the health, safety and well-being (3.7) of workers
and other relevant interested parties;
— presents a lower risk of ill health yet has a significant impact on the organization, its workers and other
relevant interested parties.
3.10
contagious disease
infectious disease (3.9) that can be transmitted from person to person
EXAMPLE Influenza, Ebola, hepatitis.
3.11
outbreak
increase in cases of an infectious disease (3.9) in excess of what is normally expected in a particular
location, community or geographical region in a specified time period
Note 1 to entry: An outbreak can affect a small and localized group or multiple groups and places and can result
in an epidemic (3.12) or pandemic (3.13).
Note 2 to entry: Two linked cases of an infectious disease can be sufficient to constitute an outbreak.
3.12
epidemic
large number of cases of a particular infectious disease (3.9), occurring at the same time in a community
or geographic region
[SOURCE: ISO 28901:2011, 3.6 modified — “infectious” has been added before “disease”, “usually
infectious” has been deleted, “particular community” has been replaced with “community or geographic
region” in the definition.]
3.13
pandemic
worldwide spread of an infectious disease (3.9)
Note 1 to entry: A pandemic is declared by the World Health Organization (WHO).
[SOURCE: ISO/PAS 45005:2020, 3.5, modified — “infectious” added before “disease” and Note 1 to entry
has been added.]
3.14
endemic infectious disease
infectious disease (3.9) either constantly present or usually prevalent in a particular geographic region
4 Context of the organization
4.1 General
The organization should obtain and maintain awareness of known and emerging infectious diseases
that can, or are likely to, significantly affect the organization or its activities.
The organization should determine external and internal issues and consider:
a) the specific hazards and related risks from infectious diseases to workers and other interested
parties who can be affected by the organization’s activities (e.g. visitors, customers, clients, service
users, the public) (see 8.1, 8.2 and 8.3);
b) if changes should be made to its operations to address the risks (see 8.4);
c) how workers can be supported to work safely (see Clauses 11 to 17).
NOTE 1 Infectious diseases can vary in occurrence, impact and severity depending on country or region.
NOTE 2 Appropriate controls can vary depending on country or region.
4.2 External issues
When determining external issues, the organization should consider:
a) emergence and/or prevalence of infectious disease within the local community (including in other
organizations and other workplaces);
b) local, regional, national and international circumstances and related legal requirements and other
requirements, and guidance (e.g. likelihood of infectious diseases being transmitted through
people, products or services moving from one place to another);
c) availability of clinical services, testing, treatments and vaccines;
d) availability of health, safety and other supplies (e.g. PPE, face coverings, hand sanitizers,
thermometers, cleaning and disinfection materials);
e) potential changes or problems in the supply chain;
f) the modes of transport workers use to travel to and from work (e.g. public transport, car, bicycle,
walking, shared transport);
g) workers travelling into regions with an endemic infectious disease or an outbreak of an infectious
disease;
h) workers' access to childcare and schooling for their children;
i) suitability of worker’s home for remote working;
j) workers’ domestic situations (e.g. living with someone who is at higher risk of contracting or
getting severely ill from infectious diseases);
k) continuity of essential services (e.g. food provision, domestic infrastructure, utilities);
l) changes in the needs and expectations, or behaviours of relevant interested parties;
m) local culture and cultural behaviours (e.g. kissing, hugging, shaking hands);
n) increased or decreased demand for the organization’s products/services.
4.3 Internal issues
4.3.1 General
When determining internal issues, the organization should consider:
a) prevalence or likelihood of an infectious disease in the organization;
b) sources of infectious agents in the workplace that can result in an infectious disease
c) ability of the organization to gain up-to-date knowledge about infectious diseases;
d) type of organization and related activities (e.g. primary production, processing, manufacturing,
services, retail, social care, training or other education, delivery or distribution);
e) number, locations and types of workplaces potentially affected (e.g. offices, factories, workshops,
warehouses, water treatment plants, vehicles, retail outlets, workers’ own homes or other people’s
homes);
f) how work is organized (e.g. changed work demands, pace of work, time pressure, shift work, travel
requirements) and how this impacts workers’ health, safety and well-being;
g) resource availability (e.g. operational, health and safety, hygiene);
h) cultural values within the organization that can affect risk controls;
i) the relationship between workers and the organization (e.g. employed, contractors, volunteers,
freelance, part-time, shift workers, remote workers);
j) specific needs of workers considered to be at higher risk for contracting or getting severely ill from
an infectious disease (e.g. workers with underlying health conditions);
k) specific needs of diverse workers (see 4.3.2);
l) language barriers and communication issues;
m) the extent to which it is possible to implement specific infection controls in a workplace or in
relation to work activities or ways of working;
n) increased worker absence (e.g. due to illness, self-isolation or quarantine requirements,
bereavement).
4.3.2 Diversity of workers and other relevant interested parties
The organization should take into account the full diversity of its workers and other relevant interested
parties when determining internal issues (see 4.3.1) relating to preventing and managing infectious
diseases. The organization should consider that individual workers and other relevant interested
parties have different needs, based on their characteristics and personal circumstances, such as:
a) gender-specific needs;
b) pregnancy or recently given birth;
c) those caring for or living with vulnerable individuals (e.g. infants, immunocompromised family
members);
d) age, taking into account both older and younger workers;
e) disabilities;
f) ethnicity, culture and faith;
g) those with underlying health conditions (e.g. immunocompromised, asthmatics).
NOTE 1 Disabilities can affect the suitability of controls for infectious diseases, including accessibility to
buildings, facilities, equipment or services. Disabilities include physical and mental impairment. People with a
disability can include wheelchair users, those with mobility, hearing or sight impairment, or with a condition or
illness that has an impact on their mental capacity.
NOTE 2 Many people have disabilities or vulnerabilities to infectious diseases, or specific needs which are not
immediately apparent (e.g. people with diabetes, respiratory conditions, heart conditions, hearing impairment).
5 Characteristics of infectious diseases
As part of the assessment of risks, the organization should take into account the characteristics of
infectious diseases that are likely to impact workers and other interested parties, so that suitable
controls can be determined (see Clause 8). Characteristics of an infectious disease include:
a) virulence of the infectious agent causing the disease;
b) likelihood of transmission;
c) incubation period;
d) time frame during which people can transmit a contagious disease;
e) length of time an infectious agent remains infectious on contaminated objects or materials;
f) symptoms related to the infectious disease;
g) potential severity of illnesses (see Table A.1);
h) sources and modes of transmission, including:
1) an infectious agent carried by another person that is spread through skin-to-skin contact,
biological waste or exchange of bodily fluids (e.g. personal care hazards, sexual interaction);
2) animals or insects that are infected with or carry an infectious agent (e.g. through touch, stings
or bites);
3) contaminated environmental sources (e.g. through water or air);
4) inhalation (e.g. mould spores, inhalation of bodily fluids from coughing);
5) ingestion (e.g. through eating contaminated food);
6) skin puncture (e.g. injections, wounds);
7) contact with a contaminated surface or object (e.g. used needles, door handles).
The organization should seek advice from:
— trusted bodies (e.g. public health authorities, disease control centres, the World Health Organization,
the International Labour Organization);
— specialists (e.g. epidemiologists, infectious disease physicians, occupational health specialists and
hygienists, public health practitioners, other infectious disease experts).
The organization should be aware that information about emerging diseases changes over time.
NOTE Some people who are infected do not show symptoms but can transmit the disease.
6 Le adership and worker participation
6.1 Leadership
Top management, and managers at all levels should demonstrate leadership to effectively manage risks
to workers and other relevant interested parties arising from infectious diseases that are, or can be, in
the workplace.
Top management should communicate to workers and other interested parties:
— how concerns about, or incidences of, infectious diseases should be reported;
— the organization’s commitment to transparency when managing infectious diseases;
— actions to take if a person has, or suspects they have, contracted an infectious disease;
— actions the organization will take to support workers and other relevant interested parties when
there is an outbreak of an infectious disease or an infectious disease incident;
— support for workers to remove themselves from work situations believed to present an imminent or
serious risk to life or health.
When an infectious disease is known to be, or can be, an issue, top management should:
a) provide adequate resources (see Clause 10) and make them available in a timely and effective
manner;
b) consult with, and encourage, participation of workers and worker representatives, where they
exist, in making decisions that affect work-related health, safety and well-being (see 6.2);
c) provide appropriate support for workers unable to work, including provision of appropriate
leave from work, paid if possible (so that concerns about pay do not lead to workers coming to a
workplace when they are unwell or potentially contagious);
d) protect workers from reprisals when reporting potential cases of illness or incidents;
e) coordinate across all parts of the organization when implementing measures to manage the risks
to workers and other relevant interested parties related to infectious diseases;
f) ensure the health and safety of workers in workplaces not under the control of the organization
(e.g. at home, in other people’s homes, workers in a mobile role, other locations) are taken into
account;
g) seek advice and information from competent and trusted bodies, specialists and sources on
managing risks to workers and other relevant interested parties, when necessary;
h) implement processes for returning to work and rehabilitation.
Managers at all levels should ensure workers have been instructed on what to do in relation to exposure
to an infectious agent (e.g. seeking medical or psychological advice) and support workers to take
appropriate actions.
6.2 Consultation and participation of workers
The organization should consult workers and encourage their participation as appropriate to facilitate
better understanding of infectious agents that can impact the organization as well as hazards and risks
related to infectious diseases and health outcomes.
Taking into account the full diversity of the workforce (see 4.3.2), the organization should:
a) promote and support participation of workers, including those with specific OH&S responsibilities,
worker representatives and subject-matter experts, where they exist, in assessing risks related to
infectious diseases and making decisions on how to manage them;
b) provide ways for workers, worker representatives, where they exist, and other relevant interested
parties to suggest improvements, including anonymously to give feedback;
c) seek feedback from workers and worker representatives, where they exist, on actions taken to
manage health, safety and well-being (e.g. meetings collaboration tools, online surveys, emails);
d) address concerns raised by workers and other relevant interested parties (including health
professionals and other experts) and provide feedback on action taken.
6.3 Roles, responsibilities and competence
While top management has ultimate accountability, top management should consider assigning specific
workers (or a single worker in a small organization) the role of implementing, maintaining, activating
or increasing health and safety controls associated with infectious diseases, assessing effectiveness,
and reporting issues.
The organization can also consider establishing an advisory group, including a top management
representative, to determine a plan for preventing and/or managing infectious diseases that can
significantly affect the organization and its activities. The advisory group can include, for example,
infectious disease experts, health and safety committee members, crisis management experts, business
continuity experts and workers or workers’ representatives where they exist.
The organization should ensure that workers are competent to perform any roles or activities relating to
infectious diseases that they are assigned. If workers are allocated new roles or tasks, the organization
should provide adequate training and support to ensure workers are competent to perform those roles.
7 Communication
7.1 General
The organization should communicate with workers and other relevant interested parties on controls
for preventing exposure to and transmission of infectious agents and managing the risks related to
an infectious disease. When an infectious disease is known to be of concern, the organization should
provide information and guidance on:
a) the characteristics of a relevant infectious disease of current concern, including potential severity,
symptoms and how it is transmitted (see Clause 5);
b) changes relating to entering or moving around a workplace;
c) changes to work times, locations, activities and work tasks;
d) changes in processes, policies, equipment and facilities that have been made or are likely to be
made;
e) changes in the availability of, or access to, facilities or functions [e.g. use of rest areas, shared
equipment, human resources (HR), information technology (IT) support].
The organization should establish who is responsible for communicating health and safety information
and guidance:
— externally, for example to suppliers, visitors, customers, workers from other organizations and
other interested parties;
— internally, to all types of workers, including new, temporary, remote and shift workers.
Communication with workers and other relevant interested parties should be two-way and encourage
ongoing conversation as well as more formal participation (see 6.2).
The organization should consider when communications about workplace changes in relation to an
incident or outbreak of infectious disease should occur. These can include:
— before first arrival at the workplace (e.g. by phone, website, intranet, email);
— on first and subs
...
INTERNATIONAL ISO
STANDARD 45006
First edition
2023-12
Occupational health and safety
management — Guidelines for
organizations on preventing,
controlling and managing infectious
diseases
Management de la santé et de la sécurité au travail — Lignes
directrices sur la prévention, le contrôle et la prise en charge des
maladies infectieuses destinées aux organismes
Reference number
© ISO 2023
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting on
the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address below
or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii
Contents Page
Foreword .v
Introduction . vi
1 Scope . 1
2 Normative references . 1
3 Terms and definitions . 1
4 Context of the organization .4
4.1 General . 4
4.2 External issues . 4
4.3 Internal issues . 5
4.3.1 General . 5
4.3.2 Diversity of workers and other relevant interested parties . 5
5 Characteristics of infectious diseases . 6
6 L eadership and worker participation . 7
6.1 Leadership . 7
6.2 Consultation and participation of workers . 7
6.3 Roles, responsibilities and competence . 8
7 Communication .8
7.1 General . 8
7.2 Methods of communication . 9
7.3 Communication with and reporting to external interested parties. 9
8 Hazards, risks and controls .9
8.1 Identification of hazards . 9
8.2 A ssessment of risks . 10
8.3 Determination of controls . 11
8.3.1 Selection of controls . 11
8.3.2 Hierarchy of controls . 11
8.3.3 Additional considerations for controls .12
8.4 P lanning of changes to controls .12
9 Psychological health and well-being .13
9.1 Psychosocial hazards and risks . 13
9.2 Controls to manage psychosocial risks . 13
10 Resources .14
11 Implementation of controls for infectious diseases .15
11.1 General . 15
11.2 Personal hygiene . 15
11.3 Work-related travel . 16
12 Implementation of controls for contagious diseases .16
12.1 General . 16
12.2 Workplaces under the control of the organization . 17
12.2.1 General workplace infection controls . 17
12.2.2 Use of common areas . 18
12.2.3 Meetings and visits to workplaces . 19
12.2.4 Deliveries . 19
12.3 Working from home . 20
12.4 Working in other people’s homes . 20
12.5 Working in multiple locations . 21
12.6 Working with the public . 22
13 Implementation of controls for non-contagious infectious diseases .22
iii
14 Implementation of controls for endemic diseases .23
15 Use of personal protective equipment and face coverings .23
15.1 General .23
15.2 Selection of appropriate protection . 24
15.2.1 General . 24
15.2.2 Protective gloves . 24
15.2.3 Face and respiratory protection . 25
16 Emergency preparedness and response .26
17 Management of suspected or confirmed cases of a relevant infectious disease .27
17.1 General . 27
17.2 Managing illness in a workplace . 27
17.2.1 General . 27
17.2.2 Occurrence of contagious disease.28
17.3 Screening, testing, contact tracing, quarantine and vaccination .28
18 Per f or m a nc e ev a lu at ion .28
18.1 General .28
18.2 M onitoring and measurement .29
18.3 Analysis and evaluation . 30
18.4 M anagement review . 30
19 Improvement .30
Annex A (informative) Examples of risk tables.32
Bibliography .34
iv
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out
through ISO technical committees. Each member body interested in a subject for which a technical
committee has been established has the right to be represented on that committee. International
organizations, governmental and non-governmental, in liaison with ISO, also take part in the work.
ISO collaborates closely with the International Electrotechnical Commission (IEC) on all matters of
electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are
described in the ISO/IEC Directives, Part 1. In particular, the different approval criteria needed for the
different types of ISO document should be noted. This document was drafted in accordance with the
editorial rules of the ISO/IEC Directives, Part 2 (see www.iso.org/directives).
ISO draws attention to the possibility that the implementation of this document may involve the use
of (a) patent(s). ISO takes no position concerning the evidence, validity or applicability of any claimed
patent rights in respect thereof. As of the date of publication of this document, ISO had not received
notice of (a) patent(s) which may be required to implement this document. However, implementers are
cautioned that this may not represent the latest information, which may be obtained from the patent
database available at www.iso.org/patents. ISO shall not be held responsible for identifying any or all
such patent rights.
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation of the voluntary nature of standards, the meaning of ISO specific terms and
expressions related to conformity assessment, as well as information about ISO's adherence to
the World Trade Organization (WTO) principles in the Technical Barriers to Trade (TBT), see
www.iso.org/iso/foreword.html.
This document was prepared by Technical Committee ISO/TC 283, Occupational health and safety
management.
Any feedback or questions on this document should be directed to the user’s national standards body. A
complete listing of these bodies can be found at www.iso.org/members.html.
v
Introduction
Infectious diseases are increasingly recognized as major challenges to health, safety and well-being.
Decisions and activities relating to the prevention and management of infectious diseases affect workers
within the organization and other people who visit a workplace, come into contact with workers or can
be affected by the organization’s activities. This document is a response to the risks that infectious
diseases present to workers and other relevant interested parties (e.g. customers, the public, suppliers,
workers from other organizations, family members and other personal contacts).
There is a broad range of infectious diseases with potential impacts on health, safety and well-being,
which can vary from very mild to very serious depending on the nature of the infectious disease. Key
characteristics of infectious diseases (see Clause 5) are a major factor in the risk posed to workers and
other relevant interested parties.
Some infectious diseases are non-contagious and infect only the individual who contracts the disease
and do not usually transmit from human to human (e.g. legionellosis or malaria), while others are
contagious and have the potential to spread from a single individual to infect others (e.g. influenza,
COVID-19, smallpox, hepatitis, salmonellosis, tuberculosis, Ebola and HIV/AIDS), up to and including a
pandemic spread of the disease.
The impact in terms of severity of infectious diseases can vary from person to person depending on
underlying health conditions (e.g. asthma, diabetes, obesity, strength of immune system) and factors
such as age, sex and socio-economic situation. Impacts can be more severe where one or more such
circumstances exist.
This document provides guidelines to prevent or reduce exposure to, and transmission of, infectious
agents and to manage risks to workers and other relevant interested parties from infectious diseases. It
supports the principle that workers should not be required to work in settings without implementation
of appropriate prevention and controls.
The guidance is generic and applicable to organizations regardless of the nature of business, service
provision, size or complexity. It recognizes that many smaller organizations do not have dedicated
departments or functions such as occupational health and safety (OH&S), facilities management, human
resources or infectious disease specialists. More detailed information for specific functions is available
from professional bodies and a wide range of national and international standards.
Organizations using ISO 45001 can use this document to improve OH&S management by relating the
relevant clauses to the PDCA cycle:
— Plan: plan what needs to be done for the organization to work safely;
— Do: do what the organization has planned to do;
— Check: see how well it is working;
— Act: take actions to improve or change controls that are not effective.
Taking a system's approach facilitates the coordination of resources and efforts and will enable
organizations to better manage the risk from infectious diseases, by ensuring they are included in
existing OH&S processes.
This document is not intended to be a single step-by-step set of recommendations. It provides guidelines
to enable ongoing continual improvement and to ensure the organization responds to incidents of
infectious diseases, including epidemics and pandemics.
This document is designed to complement ISO 45001 by providing guidelines that align with the
requirements of ISO 45001. This document can be used independently, by any organization, to improve
OH&S performance.
vi
INTERNATIONAL STANDARD ISO 45006:2023(E)
Occupational health and safety management — Guidelines
for organizations on preventing, controlling and managing
infectious diseases
1 Scope
This document gives guidelines for organizations on how to prevent or control exposure to infectious
agents at the workplace and manage the risks associated with infectious diseases that:
— present a risk of severe ill health or death and can impact the health, safety and well-being of workers
and other relevant interested parties;
— present a lower risk to health yet have a significant impact on the organization, its workers and
other relevant interested parties.
This document is applicable to organizations of all sizes and sectors.
NOTE This document does not provide comprehensive guidance to those parts of an organization that
implement mandated infection controls such as hospitals and medical or biological laboratories because there
is an inherent potential for exposure to infectious diseases. Applicable legislation and guidance are provided
by government, regulators and health authorities for specific infection controls for the protection of workers in
such settings and for work activities on or with pathogenic microorganisms.
2 Normative references
The following documents are referred to in the text in such a way that some or all of their content
constitutes requirements of this document. For dated references, only the edition cited applies. For
undated references, the latest edition of the referenced document (including any amendments) applies.
ISO 45001:2018, Occupational health and safety management systems — Requirements with guidance for
use
3 Terms and definitions
For the purposes of this document, the terms and definitions given in ISO 45001 and the following apply.
ISO and IEC maintain terminology databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https:// www .iso .org/ obp
— IEC Electropedia: available at https:// www .electropedia .org/
3.1
workplace
place where a person needs to be or to go for work purposes
Note 1 to entry: The organization’s responsibilities for the workplace depend on the degree of control over the
workplace.
Note 2 to entry: Workplaces can be inside or outside and include the worker’s own home, other people’s homes,
personal vehicles, vehicles provided by the organization, other organizations’ facilities and public spaces.
[SOURCE: ISO 45001:2018, 3.6, modified — “under the control of the organization” has been deleted
from the definition, “under the OH&S management system” has been deleted from Note 1 to entry and
Note 2 to entry has been added.]
3.2
legal requirements and other requirements
legal requirements that an organization has to comply with and other requirements that an organization
has to or chooses to comply with
[SOURCE: ISO 45001:2018, 3.9, modified — Notes 1, 2 and 3 to entry have been deleted.]
3.3
top management
person or group of people who directs and controls an organization at the highest level
[SOURCE: ISO 45001:2018, 3.12, modified — Notes 1, 2 and 3 to entry have been deleted.]
3.4
incident
occurrence arising out of, or in the course of, work that can or does result in injury and ill health
Note 1 to entry: In this document, “injury and ill health” refers to contracting an infectious disease (3.8) or any
identifiable, adverse physical or psychological condition arising from or associated with an infectious disease.
[SOURCE: ISO 45001:2018, 3.35, modified — Note 1 to entry has been replaced, and Notes 2 and 3 to
entry have been deleted.]
3.5
personal protective equipment
PPE
device or appliance designed to be worn by an individual for their protection against one or more health
and safety hazards
Note 1 to entry: PPE includes, but is not limited to, gowns, gloves, respirators, safety glasses, helmets and goggles.
Note 2 to entry: While generally not considered PPE, masks, and other face coverings (3.6) can provide a level of
protection for the user in addition to their primary purpose as a public health measure to control the spread of
transmission and infection.
Note 3 to entry: In many countries, PPE is required to conform to national regulations.
[SOURCE: ISO 15384:2018, 3.12, modified — “or held” have been deleted after “worn” and “their” has
been added before “protection” in the definition, and Notes 1, 2 and 3 to entry have been added.]
3.6
face covering
facepiece that covers the mouth, nose and chin
EXAMPLE ‘community masks’, ‘hygiene masks’, ‘barrier masks’, and ‘comfort masks’ are all examples of face
coverings.
Note 1 to entry: Face coverings in the context of this document are not considered to be personal protective
equipment (PPE) (3.5) or a medical device.
3.7
well-being
fulfilment of the physical, mental and cognitive needs and expectations of a worker related to their
work
Note 1 to entry: Well-being can also contribute to the quality of life outside of work.
Note 2 to entry: Well-being relates to all aspects of working life, including work organization, social factors at
work, work environment, equipment and hazardous tasks.
[SOURCE: ISO 45003:2021, 3.2, modified — “at work” has been deleted after “well-being” from the term
and Notes 1 and 2 to entry have been added.]
3.8
common area
space and amenity provided for the use of more than one person
EXAMPLE Canteens, lifts/elevators, stairs, reception areas, meeting rooms, areas of worship, toilets,
gardens, fire escapes, kitchens, fitness facilities, store rooms, laundry facilities.
Note 1 to entry: Common areas can include spaces and amenities used by more than one organization.
Note 2 to entry: Common areas can include spaces and amenities where people are working.
[SOURCE: ISO/PAS 45005:2020, 3.11, modified — the term "common areas" has been changed to
"common area", "spaces and amenities" has been changed to "space and amenity" in the definition, and
Notes 1 and 2 to entry have been added.]
3.9
infectious disease
condition caused by agents such as bacteria, viruses, prion, parasites or fungi that can spread, directly
or indirectly, and that can result in ill-health
Note 1 to entry: In this document, “infectious disease” refers to a disease that:
— presents a risk of severe ill health or death and can impact the health, safety and well-being (3.7) of workers
and other relevant interested parties;
— presents a lower risk of ill health yet has a significant impact on the organization, its workers and other
relevant interested parties.
3.10
contagious disease
infectious disease (3.9) that can be transmitted from person to person
EXAMPLE Influenza, Ebola, hepatitis.
3.11
outbreak
increase in cases of an infectious disease (3.9) in excess of what is normally expected in a particular
location, community or geographical region in a specified time period
Note 1 to entry: An outbreak can affect a small and localized group or multiple groups and places and can result
in an epidemic (3.12) or pandemic (3.13).
Note 2 to entry: Two linked cases of an infectious disease can be sufficient to constitute an outbreak.
3.12
epidemic
large number of cases of a particular infectious disease (3.9), occurring at the same time in a community
or geographic region
[SOURCE: ISO 28901:2011, 3.6 modified — “infectious” has been added before “disease”, “usually
infectious” has been deleted, “particular community” has been replaced with “community or geographic
region” in the definition.]
3.13
pandemic
worldwide spread of an infectious disease (3.9)
Note 1 to entry: A pandemic is declared by the World Health Organization (WHO).
[SOURCE: ISO/PAS 45005:2020, 3.5, modified — “infectious” added before “disease” and Note 1 to entry
has been added.]
3.14
endemic infectious disease
infectious disease (3.9) either constantly present or usually prevalent in a particular geographic region
4 Context of the organization
4.1 General
The organization should obtain and maintain awareness of known and emerging infectious diseases
that can, or are likely to, significantly affect the organization or its activities.
The organization should determine external and internal issues and consider:
a) the specific hazards and related risks from infectious diseases to workers and other interested
parties who can be affected by the organization’s activities (e.g. visitors, customers, clients, service
users, the public) (see 8.1, 8.2 and 8.3);
b) if changes should be made to its operations to address the risks (see 8.4);
c) how workers can be supported to work safely (see Clauses 11 to 17).
NOTE 1 Infectious diseases can vary in occurrence, impact and severity depending on country or region.
NOTE 2 Appropriate controls can vary depending on country or region.
4.2 External issues
When determining external issues, the organization should consider:
a) emergence and/or prevalence of infectious disease within the local community (including in other
organizations and other workplaces);
b) local, regional, national and international circumstances and related legal requirements and other
requirements, and guidance (e.g. likelihood of infectious diseases being transmitted through
people, products or services moving from one place to another);
c) availability of clinical services, testing, treatments and vaccines;
d) availability of health, safety and other supplies (e.g. PPE, face coverings, hand sanitizers,
thermometers, cleaning and disinfection materials);
e) potential changes or problems in the supply chain;
f) the modes of transport workers use to travel to and from work (e.g. public transport, car, bicycle,
walking, shared transport);
g) workers travelling into regions with an endemic infectious disease or an outbreak of an infectious
disease;
h) workers' access to childcare and schooling for their children;
i) suitability of worker’s home for remote working;
j) workers’ domestic situations (e.g. living with someone who is at higher risk of contracting or
getting severely ill from infectious diseases);
k) continuity of essential services (e.g. food provision, domestic infrastructure, utilities);
l) changes in the needs and expectations, or behaviours of relevant interested parties;
m) local culture and cultural behaviours (e.g. kissing, hugging, shaking hands);
n) increased or decreased demand for the organization’s products/services.
4.3 Internal issues
4.3.1 General
When determining internal issues, the organization should consider:
a) prevalence or likelihood of an infectious disease in the organization;
b) sources of infectious agents in the workplace that can result in an infectious disease
c) ability of the organization to gain up-to-date knowledge about infectious diseases;
d) type of organization and related activities (e.g. primary production, processing, manufacturing,
services, retail, social care, training or other education, delivery or distribution);
e) number, locations and types of workplaces potentially affected (e.g. offices, factories, workshops,
warehouses, water treatment plants, vehicles, retail outlets, workers’ own homes or other people’s
homes);
f) how work is organized (e.g. changed work demands, pace of work, time pressure, shift work, travel
requirements) and how this impacts workers’ health, safety and well-being;
g) resource availability (e.g. operational, health and safety, hygiene);
h) cultural values within the organization that can affect risk controls;
i) the relationship between workers and the organization (e.g. employed, contractors, volunteers,
freelance, part-time, shift workers, remote workers);
j) specific needs of workers considered to be at higher risk for contracting or getting severely ill from
an infectious disease (e.g. workers with underlying health conditions);
k) specific needs of diverse workers (see 4.3.2);
l) language barriers and communication issues;
m) the extent to which it is possible to implement specific infection controls in a workplace or in
relation to work activities or ways of working;
n) increased worker absence (e.g. due to illness, self-isolation or quarantine requirements,
bereavement).
4.3.2 Diversity of workers and other relevant interested parties
The organization should take into account the full diversity of its workers and other relevant interested
parties when determining internal issues (see 4.3.1) relating to preventing and managing infectious
diseases. The organization should consider that individual workers and other relevant interested
parties have different needs, based on their characteristics and personal circumstances, such as:
a) gender-specific needs;
b) pregnancy or recently given birth;
c) those caring for or living with vulnerable individuals (e.g. infants, immunocompromised family
members);
d) age, taking into account both older and younger workers;
e) disabilities;
f) ethnicity, culture and faith;
g) those with underlying health conditions (e.g. immunocompromised, asthmatics).
NOTE 1 Disabilities can affect the suitability of controls for infectious diseases, including accessibility to
buildings, facilities, equipment or services. Disabilities include physical and mental impairment. People with a
disability can include wheelchair users, those with mobility, hearing or sight impairment, or with a condition or
illness that has an impact on their mental capacity.
NOTE 2 Many people have disabilities or vulnerabilities to infectious diseases, or specific needs which are not
immediately apparent (e.g. people with diabetes, respiratory conditions, heart conditions, hearing impairment).
5 Characteristics of infectious diseases
As part of the assessment of risks, the organization should take into account the characteristics of
infectious diseases that are likely to impact workers and other interested parties, so that suitable
controls can be determined (see Clause 8). Characteristics of an infectious disease include:
a) virulence of the infectious agent causing the disease;
b) likelihood of transmission;
c) incubation period;
d) time frame during which people can transmit a contagious disease;
e) length of time an infectious agent remains infectious on contaminated objects or materials;
f) symptoms related to the infectious disease;
g) potential severity of illnesses (see Table A.1);
h) sources and modes of transmission, including:
1) an infectious agent carried by another person that is spread through skin-to-skin contact,
biological waste or exchange of bodily fluids (e.g. personal care hazards, sexual interaction);
2) animals or insects that are infected with or carry an infectious agent (e.g. through touch, stings
or bites);
3) contaminated environmental sources (e.g. through water or air);
4) inhalation (e.g. mould spores, inhalation of bodily fluids from coughing);
5) ingestion (e.g. through eating contaminated food);
6) skin puncture (e.g. injections, wounds);
7) contact with a contaminated surface or object (e.g. used needles, door handles).
The organization should seek advice from:
— trusted bodies (e.g. public health authorities, disease control centres, the World Health Organization,
the International Labour Organization);
— specialists (e.g. epidemiologists, infectious disease physicians, occupational health specialists and
hygienists, public health practitioners, other infectious disease experts).
The organization should be aware that information about emerging diseases changes over time.
NOTE Some people who are infected do not show symptoms but can transmit the disease.
6 Le adership and worker participation
6.1 Leadership
Top management, and managers at all levels should demonstrate leadership to effectively manage risks
to workers and other relevant interested parties arising from infectious diseases that are, or can be, in
the workplace.
Top management should communicate to workers and other interested parties:
— how concerns about, or incidences of, infectious diseases should be reported;
— the organization’s commitment to transparency when managing infectious diseases;
— actions to take if a person has, or suspects they have, contracted an infectious disease;
— actions the organization will take to support workers and other relevant interested parties when
there is an outbreak of an infectious disease or an infectious disease incident;
— support for workers to remove themselves from work situations believed to present an imminent or
serious risk to life or health.
When an infectious disease is known to be, or can be, an issue, top management should:
a) provide adequate resources (see Clause 10) and make them available in a timely and effective
manner;
b) consult with, and encourage, participation of workers and worker representatives, where they
exist, in making decisions that affect work-related health, safety and well-being (see 6.2);
c) provide appropriate support for workers unable to work, including provision of appropriate
leave from work, paid if possible (so that concerns about pay do not lead to workers coming to a
workplace when they are unwell or potentially contagious);
d) protect workers from reprisals when reporting potential cases of illness or incidents;
e) coordinate across all parts of the organization when implementing measures to manage the risks
to workers and other relevant interested parties related to infectious diseases;
f) ensure the health and safety of workers in workplaces not under the control of the organization
(e.g. at home, in other people’s homes, workers in a mobile role, other locations) are taken into
account;
g) seek advice and information from competent and trusted bodies, specialists and sources on
managing risks to workers and other relevant interested parties, when necessary;
h) implement processes for returning to work and rehabilitation.
Managers at all levels should ensure workers have been instructed on what to do in relation to exposure
to an infectious agent (e.g. seeking medical or psychological advice) and support workers to take
appropriate actions.
6.2 Consultation and participation of workers
The organization should consult workers and encourage their participation as appropriate to facilitate
better understanding of infectious agents that can impact the organization as well as hazards and risks
related to infectious diseases and health outcomes.
Taking into account the full diversity of the workforce (see 4.3.2), the organization should:
a) promote and support participation of workers, including those with specific OH&S responsibilities,
worker representatives and subject-matter experts, where they exist, in assessing risks related to
infectious diseases and making decisions on how to manage them;
b) provide ways for workers, worker representatives, where they exist, and other relevant interested
parties to suggest improvements, including anonymously to give feedback;
c) seek feedback from workers and worker representatives, where they exist, on actions taken to
manage health, safety and well-being (e.g. meetings collaboration tools, online surveys, emails);
d) address concerns raised by workers and other relevant interested parties (including health
professionals and other experts) and provide feedback on action taken.
6.3 Roles, responsibilities and competence
While top management has ultimate accountability, top management should consider assigning specific
workers (or a single worker in a small organization) the role of implementing, maintaining, activating
or increasing health and safety controls associated with infectious diseases, assessing effectiveness,
and reporting issues.
The organization can also consider establishing an advisory group, including a top management
representative, to determine a plan for preventing and/or managing infectious diseases that can
significantly affect the organization and its activities. The advisory group can include, for example,
infectious disease experts, health and safety committee members, crisis management experts, business
continuity experts and workers or workers’ representatives where they exist.
The organization should ensure that workers are competent to perform any roles or activities relating to
infectious diseases that they are assigned. If workers are allocated new roles or tasks, the organization
should provide adequate training and support to ensure workers are competent to perform those roles.
7 Communication
7.1 General
The organization should communicate with workers and other relevant interested parties on controls
for preventing exposure to and transmission of infectious agents and managing the risks related to
an infectious disease. When an infectious disease is known to be of concern, the organization should
provide information and guidance on:
a) the characteristics of a relevant infectious disease of current concern, including potential severity,
symptoms and how it is transmitted (see Clause 5);
b) changes relating to entering or moving around a workplace;
c) changes to work times, locations, activities and work tasks;
d) changes in processes, policies, equipment and facilities that have been made or are likely to be
made;
e) changes in the availability of, or access to, facilities or functions [e.g. use of rest areas, shared
equipment, human resources (HR), information technology (IT) support].
The organization should establish who is responsible for communicating health and safety information
and guidance:
— externally, for example to suppliers, visitors, customers, workers from other organizations and
other interested parties;
— internally, to all types of workers, including new, temporary, remote and shift workers.
Communication with workers and other relevant interested parties should be two-way and encourage
ongoing conversation as well as more formal participation (see 6.2).
The organization should consider when communications about workplace changes in relation to an
incident or outbreak of infectious disease should occur. These can include:
— before first arrival at the workplace (e.g. by phone, website, intranet, email);
— on first and subsequent arrivals at the workplace (e.g. signs, posters, screens, announcements);
— when work is being performed (e.g. signs, posters, screens, announcements);
— when infectious disease control measures are no longer necessary or can be relaxed.
7.2 Methods of communication
The organization should:
a) use a combination of formal and informal communication methods (e.g. intranet, website, email,
social media, signs, images, symbols, phone calls, text messages, audio announcements, video)
so messages are accessible and can be understood by all relevant interested parties, including
customers, clients and the public, taking into account the needs of people with disabilities, non-
native speakers and people with differing levels of literacy;
b) ensure standardized symbols are used in visual communications, including signs, wherever
possible, to avoid misinterpretation;
c) communicate relevant information about operational changes, health and safety measures, and
controls to workers and other relevant interested parties, including the public (see 12.6);
d) review communications frequently to ensure they are updated, clear and effective, and take action
if issues
...
NORMA ISO
INTERNACIONAL 45006
Traducción oficial
Primera edición
2023-12
Official translation
Traduction officielle
Gestión de la seguridad y salud en
el trabajo — Directrices para las
organizaciones sobre prevención,
control y gestión de enfermedades
infecciosas
Occupational health and safety management — Guidelines for
organizations on preventing, controlling and managing infectious
diseases
Management de la santé et de la sécurité au travail — Lignes
directrices sur la prévention, le contrôle et la prise en charge des
maladies infectieuses destinées aux organismes
Publicado por la Secretaría Central de ISO en Ginebra, Suiza,
como traducción oficial en español avalada por el Translation
Management Group, que ha certificado la conformidad en relación
con las versiones inglesa y francesa.
Número de referencia
DOCUMENTO PROTEGIDO POR COPYRIGHT
© ISO 2023
Reservados los derechos de reproducción. Salvo prescripción diferente, no podrá reproducirse ni utilizarse ninguna parte de
esta publicación bajo ninguna forma y por ningún medio, electrónico o mecánico, incluidos el fotocopiado, o la publicación en
Internet o una Intranet, sin la autorización previa por escrito. La autorización puede solicitarse a ISO en la siguiente dirección o al
organismo miembro de ISO en el país solicitante.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Email: copyright@iso.org
Website: www.iso.org
Publicado en Suiza
Version espanola publicada en 2024
Traducción oficial/Official translation/Traduction officielle
ii
Índice Página
Prólogo .v
Prólogo de la versión en español. vi
Introducción .vii
1 Objeto y campo de aplicación . 1
2 Referencias normativas . 1
3 Términos y definiciones .1
4 Contexto de la organización . 4
4.1 Generalidades . 4
4.2 Cuestiones externas . 4
4.3 Cuestiones internas . 5
4.3.1 Generalidades . 5
4.3.2 Diversidad de trabajadores y otras partes interesadas pertinentes . 6
5 Características de las enfermedades infecciosas . 6
6 Liderazgo y participación de los trabajadores . 7
6.1 Liderazgo . 7
6.2 Consulta y participación de los trabajadores . 8
6.3 Roles, responsabilidades y competencia . 9
7 Comunicación . 9
7.1 Generalidades . 9
7.2 Métodos de comunicación . 10
7.3 Comunicar e informar a partes interesadas externas. 10
8 Peligros, riesgos y controles .10
8.1 Identificación de peligros . 10
8.2 Evaluación de riesgos . 11
8.3 Determinación de los controles .12
8.3.1 Selección de controles.12
8.3.2 Jerarquía de controles . 13
8.3.3 Consideraciones adicionales para los controles .13
8.4 Planificación de cambios en los controles . 13
9 Salud psicológica y bienestar .14
9.1 Peligros y riesgos psicosociales . 14
9.2 Controles para gestionar los riesgos psicosociales . 15
10 Recursos .15
11 Implementación de controles para enfermedades infecciosas .16
11.1 Generalidades . 16
11.2 Higiene personal . 16
11.3 Viajes relacionados con el trabajo . 17
12 Implementación de controles para las enfermedades contagiosas .18
12.1 Generalidades . 18
12.2 Lugares de trabajo bajo el control de la organización . 18
12.2.1 Controles generales de infecciones en el lugar de trabajo . 18
12.2.2 Uso de áreas comunes . 20
12.2.3 Reuniones y visitas a los lugares de trabajo . 21
12.2.4 Repartos . 21
12.3 Trabajar desde el hogar. 22
12.4 Trabajar en el hogar de otras personas . 22
12.5 Trabajar en múltiples ubicaciones . 23
12.6 Trabajar con el público . 24
Traducción oficial/Official translation/Traduction officielle
iii
13 Implementación de controles de enfermedades infecciosas no contagiosas .24
14 Implementación de controles de enfermedades endémicas .25
15 Uso de equipo de protección personal y de protectores faciales .26
15.1 Generalidades .26
15.2 Selección de la protección adecuada . 26
15.2.1 Generalidades .26
15.2.2 Guantes protectores . 27
15.2.3 Protección facial y respiratoria . 27
16 Preparación y respuesta ante emergencias .28
17 Gestión de casos sospechosos o confirmados de una enfermedad infecciosa
relevante .29
17.1 Generalidades .29
17.2 Gestión de enfermedades en el lugar de trabajo .30
17.2.1 Generalidades .30
17.2.2 Ocurrencia de enfermedades contagiosas.30
17.3 Tamizaje, pruebas, rastreo de contactos, cuarentena y vacunación . 31
18 Evaluación del desempeño .31
18.1 Generalidades . 31
18.2 Seguimiento y medición . 32
18.3 Análisis y evaluación .33
18.4 Revisión por la dirección .33
19 Mejora .33
Anexo A (informativo) Ejemplos de tablas de riesgo .35
Bibliografía.38
Traducción oficial/Official translation/Traduction officielle
iv
Prólogo
ISO (Organización Internacional de Normalización) es una federación mundial de organismos
nacionales de normalización (organismos miembros de ISO). El trabajo de elaboración de las Normas
Internacionales se lleva a cabo normalmente a través de los comités técnicos de ISO. Cada organismo
miembro interesado en una materia para la cual se haya establecido un comité técnico, tiene el derecho
de estar representado en dicho comité. Las organizaciones internacionales, gubernamentales y no
gubernamentales, vinculadas con ISO, también participan en el trabajo. ISO colabora estrechamente
con la Comisión Electrotécnica Internacional (IEC) en todos los temas de normalización electrotécnica.
En la Parte 1 de las Directivas ISO/IEC se describen los procedimientos utilizados para desarrollar este
documento y aquellos previstos para su mantenimiento posterior. En particular debería tomarse nota
de los diferentes criterios de aprobación necesarios para los distintos tipos de documentos ISO. Este
documento ha sido redactado de acuerdo con las reglas editoriales de la Parte 2 de las Directivas ISO/
IEC (véase www.iso.org/directives).
ISO llama la atención sobre la posibilidad de que la implementación de este documento pueda conllevar
el uso de una o varias patentes. ISO no se posiciona respecto a la evidencia, validez o aplicabilidad de los
derechos de patente reivindicados. A la fecha de publicación de este documento, ISO no había recibido
notificación de que una o varias patentes pudieran ser necesarias para su implementación. No obstante,
se advierte a los usuarios que esta puede no ser la información más reciente, la cual puede obtenerse
de la base de datos de patentes disponible en www.iso.org/patents. ISO no será responsable de la
identificación de parte o la totalidad de dichos derechos de patente.
Cualquier nombre comercial utilizado en este documento es información que se proporciona para
comodidad del usuario y no constituye una recomendación.
Para una explicación de la naturaleza voluntaria de las normas, el significado de los términos específicos
de ISO y las expresiones relacionadas con la evaluación de la conformidad, así como la información
acerca de la adhesión de ISO a los principios de la Organización Mundial del Comercio (OMC) respecto a
los Obstáculos Técnicos al Comercio (OTC), véase www.iso.org/iso/foreword.html.
Este documento ha sido elaborado por el Comité Técnico ISO/TC 283, Sistemas de gestión de la seguridad
y salud en el trabajo.
Cualquier comentario o pregunta sobre este documento deberían dirigirse al organismo nacional de
normalización del usuario. En www.iso.org/members.html se puede encontrar un listado completo de
estos organismos.
Traducción oficial/Official translation/Traduction officielle
v
Prólogo de la versión en español
Este documento ha sido traducido por el Grupo de Trabajo Spanish Translation Task Force (STTF) del
Comité Técnico ISO/TC 283, Sistemas de gestión de la seguridad y salud en el trabajo, en el que participan
representantes de los organismos nacionales de normalización y otras partes interesadas, para lograr
la unificación de la terminología en lengua española en el ámbito de la gestión de la seguridad y salud en
el trabajo.
Este documento ha sido validado por el ISO/TMBG/Spanish Translation Management Group (STMG)
conformado por los siguientes países: Argentina, Bolivia, Chile, Colombia, Costa Rica, Cuba, Ecuador,
El Salvador, España, Guatemala, Honduras, República Dominicana, México, Panamá, Paraguay, Perú y
Uruguay.
Traducción oficial/Official translation/Traduction officielle
vi
Introducción
Las enfermedades infecciosas son cada vez más reconocidas como desafíos importantes para la salud,
la seguridad y el bienestar. Las decisiones y actividades relacionadas con la prevención y gestión de
enfermedades infecciosas afectan a los trabajadores dentro de la organización y a otras personas que
visitan un lugar de trabajo, entran en contacto con los trabajadores o pueden verse afectadas por las
actividades de la organización. Este documento es una respuesta a los riesgos que las enfermedades
infecciosas presentan para los trabajadores y otras partes interesadas pertinentes (por ejemplo,
clientes, público, proveedores, trabajadores de otras organizaciones, familiares y otros contactos
personales).
Existe una amplia gama de enfermedades infecciosas con potenciales impactos en la salud, la seguridad y
el bienestar, que pueden variar desde muy leves hasta muy graves según la naturaleza de la enfermedad
infecciosa. Las características clave de las enfermedades infecciosas (véase el Capítulo 5) son un factor
importante en el riesgo que representan para los trabajadores y otras partes interesadas pertinentes.
Algunas enfermedades infecciosas no son contagiosas e infectan solo a la persona que contrae la
enfermedad y generalmente no se transmiten de humano a humano (por ejemplo, legionelosis o malaria),
mientras que otras son contagiosas y tienen el potencial de propagarse desde una única persona para
infectar a otros (por ejemplo, gripe, COVID-19, viruela, hepatitis, salmonelosis, tuberculosis, ébola y
VIH/sida), incluso hasta una propagación pandémica de la enfermedad.
El impacto en términos de gravedad de las enfermedades infecciosas puede variar de persona a persona
dependiendo de los problemas de salud subyacentes (por ejemplo, asma, diabetes, obesidad, fortaleza
del sistema inmunológico) y factores como la edad, el sexo y la situación socioeconómica. Los impactos
pueden ser más graves cuando existen una o más de esas circunstancias.
Este documento proporciona directrices para prevenir o reducir la exposición y la transmisión de
agentes infecciosos y para gestionar los riesgos de enfermedades infecciosas para los trabajadores
y otras partes interesadas pertinentes. Respalda el principio de que no se debería requerir a los
trabajadores que trabajen en entornos sin la implementación de una apropiada prevención y de
controles.
Las orientaciones son genéricas y aplicables a las organizaciones independientemente de la naturaleza
del negocio, la provisión de servicios, el tamaño o la complejidad. Reconoce que muchas organizaciones
más pequeñas no tienen departamentos o funciones específicos, como seguridad y salud en el trabajo
(SST), gestión de instalaciones, recursos humanos o especialistas en enfermedades infecciosas.
Información más detallada para funciones específicas está disponible en organismos profesionales y en
una amplia gama de normas nacionales e internacionales.
Las organizaciones que utilizan la Norma ISO 45001 pueden utilizar este documento para mejorar la
gestión de la SST relacionando los capítulos pertinentes con el ciclo Planificar-Hacer-Verificar-Actuar
(PHVA):
— Planificar: planificar lo que se debería hacer para que la organización funcione de manera segura.
— Hacer: hacer lo que la organización ha planeado hacer.
— Verificar: ver qué tan bien está funcionando.
— Actuar: tomar acciones para mejorar o cambiar los controles que no son eficaces.
Adoptar un enfoque de sistema facilita la coordinación de recursos y esfuerzos y posibilitará a las
organizaciones gestionar mejor el riesgo derivado de enfermedades infecciosas, asegurando que están
incluidas en los procesos de la SST existentes.
Este documento no pretende ser un único conjunto de recomendaciones paso a paso. Proporciona
directrices para posibilitar la mejora continua y asegurar que la organización responda a incidentes de
enfermedades infecciosas, incluidas epidemias y pandemias.
Traducción oficial/Official translation/Traduction officielle
vii
Este documento está diseñado para complementar la Norma ISO 45001 proporcionando directrices
que se alinean con los requisitos de la Norma ISO 45001. Este documento puede ser utilizado de forma
independiente, por cualquier organización, para mejorar el desempeño de la SST.
Traducción oficial/Official translation/Traduction officielle
viii
NORMA INTERNACIONAL ISO 45006:2023 (traducción oficial)
Gestión de la seguridad y salud en el trabajo — Directrices
para las organizaciones sobre prevención, control y gestión
de enfermedades infecciosas
1 Objeto y campo de aplicación
Este documento proporciona directrices para las organizaciones sobre cómo prevenir o controlar
la exposición a agentes infecciosos en el lugar de trabajo y gestionar los riesgos asociados con
enfermedades infecciosas que:
— presentan un riesgo de deterioro grave de la salud o muerte y puede afectar a la salud, la seguridad
y el bienestar de los trabajadores y otras partes interesadas pertinentes;
— presentan un menor riesgo para la salud, pero tienen un impacto significativo en la organización,
sus trabajadores y otras partes interesadas pertinentes.
Este documento es aplicable a organizaciones de todos los tamaños y sectores.
NOTA Este documento no proporciona una orientación integral para aquellas partes de una organización
que implementan controles obligatorios de infecciones, como hospitales y laboratorios médicos o biológicos,
porque existe un potencial inherente de exposición a enfermedades infecciosas. La legislación y orientación
aplicables son proporcionadas por el gobierno, las autoridades reglamentarias y las autoridades sanitarias para
controles de infecciones específicos para la protección de los trabajadores en dichos entornos y para actividades
de trabajo sobre o con microorganismos patógenos.
2 Referencias normativas
Los siguientes documentos se referencian en el texto de tal forma que parte o la totalidad de su
contenido constituyen requisitos de este documento. Para las referencias con fecha, sólo aplica la
edición citada. Para las referencias sin fecha se aplica la última edición del documento de referencia
(incluyendo cualquier modificación).
ISO 45001:2018, Sistemas de gestión de la seguridad y salud en el trabajo — Requisitos con orientación
para su uso
3 Términos y definiciones
Para los fines de este documento, se aplican los términos y definiciones incluidos en la Norma ISO 45001
además de los siguientes,
ISO e IEC mantienen bases de datos terminológicas para su utilización en normalización en las siguientes
direcciones:
— Plataforma de búsqueda en línea de ISO: disponible en https:// www .iso .org/ obp
— Electropedia de IEC: disponible en https:// www .electropedia .org/
3.1
lugar de trabajo
lugar donde una persona necesita estar o ir por razones de trabajo
Nota 1 a la entrada: Las responsabilidades de la organización para el lugar de trabajo dependen del grado de
control sobre el lugar de trabajo.
Traducción oficial/Official translation/Traduction officielle
Nota 2 a la entrada: Los lugares de trabajo pueden ser interiores o exteriores e incluyen el propio hogar del
trabajador, el hogar de otras personas, vehículos personales, vehículos proporcionados por la organización,
instalaciones de otras organizaciones y espacios públicos.
[FUENTE: ISO 45001:2018, 3.6, modificada — "bajo el control de la organización" se eliminó de la
definición, "bajo el sistema de gestión de la SST" se eliminó de la Nota 1 a la entrada y se agregó la
Nota 2 a la entrada.]
3.2
requisitos legales y otros requisitos
requisitos legales que una organización tiene que cumplir y otros requisitos que una organización tiene
que cumplir o que elige cumplir
[FUENTE: ISO 45001:2018, 3.9, modificada — se eliminaron las Notas 1, 2 y 3 a la entrada.]
3.3
alta dirección
persona o grupo de personas que dirige y controla una organización al más alto nivel
[FUENTE: ISO 45001:2018, 3.12, modificada — se eliminaron las Notas 1, 2 y 3 a la entrada.]
3.4
incidente
suceso que surge del trabajo o en el transcurso del trabajo que podría tener o tiene como resultado
lesiones y deterioro de la salud
Nota 1 a la entrada: En este documento, "lesiones y deterioro de la salud" se refiere a contraer una enfermedad
infecciosa (3.9) o cualquier condición física o psicológica adversa identificable que surja o esté asociada con una
enfermedad infecciosa.
[FUENTE: ISO 45001:2018, 3.35, modificada — se reemplazó la Nota 1 a la entrada y se eliminaron las
Notas 2 y 3 a la entrada.]
3.5
equipo de protección personal
EPP
dispositivo o equipo diseñado para ser llevado puesto por una persona para su protección contra uno o
más peligros para la seguridad y salud
Nota 1 a la entrada: El EPP incluye, entre otros, batas, guantes, respiradores, gafas de seguridad, cascos y
protección ocular.
Nota 2 a la entrada: Si bien generalmente no se consideran EPP, las mascarillas y otros protectores faciales (3.6)
pueden proporcionar un nivel de protección para el usuario además de su propósito principal como medida de
salud pública para controlar la propagación de la transmisión y la infección.
Nota 3 a la entrada: En muchos países, se requiere que el EPP cumpla con las regulaciones nacionales.
[FUENTE: ISO 15384:2018, 3.12, modificada — "o ser sostenido" se eliminó después de "ser llevado
puesto" y se agregó "su" antes de "protección" en la definición, y se agregaron las Notas 1, 2 y 3 a la
entrada.]
3.6
protector facial
pieza facial que cubre la boca, la nariz y la barbilla
EJEMPLO Las "mascarillas comunitarias", las "mascarillas higiénicas", las "mascarillas barrera" y las
"mascarillas de confort" son ejemplos de protectores faciales.
Nota 1 a la entrada: Los protectores faciales en el contexto de este documento no se consideran equipo de
protección personal (EPP) (3.5) o un dispositivo médico.
Traducción oficial/Official translation/Traduction officielle
3.7
bienestar
satisfacción de las necesidades y expectativas físicas, mentales, y cognitivas de un trabajador
relacionadas con su trabajo
Nota 1 a la entrada: El bienestar también puede contribuir a la calidad de vida fuera del trabajo.
Nota 2 a la entrada: El bienestar se relaciona con todos los aspectos de la vida laboral, incluida la organización del
trabajo, los factores sociales en el trabajo, el entorno de trabajo, los equipos y las tareas peligrosas.
[FUENTE: ISO 45003:2021, 3.2, modificada — En el término, se eliminó "en el trabajo" después de
"bienestar", y se agregaron las Notas 1 y 2 a la entrada.]
3.8
área común
espacio y servicio proporcionados para el uso de más de una persona
EJEMPLO Comedores, ascensores/elevadores, escaleras, áreas de recepción, salas de reuniones, áreas de
culto, aseos, jardines, salidas de emergencia, cocinas, gimnasios, almacenes, lavanderías.
Nota 1 a la entrada: Las áreas comunes pueden incluir espacios y servicios utilizados por más de una organización.
Nota 2 a la entrada: Las áreas comunes pueden incluir espacios y servicios donde las personas trabajan.
[FUENTE: ISO/PAS 45005:2020, 3.11, modificada — el término "áreas comunes" se cambió a "área
común", en la definición se cambió "espacios y servicios" a "espacio y servicio", y se agregaron las
Notas 1 y 2 a la entrada.]
3.9
enfermedad infecciosa
problema causado por agentes como bacterias, virus, priones, parásitos u hongos que pueden
propagarse, directa o indirectamente, y que pueden provocar deterioro de la salud
Nota 1 a la entrada: En este documento, "enfermedad infecciosa" se refiere a una enfermedad que:
— presenta un riesgo de deterioro grave de la salud o muerte y puede afectar a la seguridad, la salud y el bienestar
(3.7) de los trabajadores y otras partes interesadas pertinentes;
— presenta un menor riesgo de deterioro de salud, pero tiene un impacto significativo en la organización, sus
trabajadores y otras partes interesadas pertinentes.
3.10
enfermedad contagiosa
enfermedad infecciosa (3.9) que puede transmitirse de persona a persona
EJEMPLO Gripe, ébola, hepatitis.
3.11
brote
aumento de casos de una enfermedad infecciosa (3.9) que excede a lo que normalmente se espera en un
lugar, comunidad o región geográfica en particular en un periodo de tiempo específico
Nota 1 a la entrada: Un brote puede afectar a un grupo pequeño y localizado o a múltiples grupos y lugares y
puede resultar en una epidemia (3.12) o una pandemia (3.13).
Nota 2 a la entrada: Dos casos relacionados de una enfermedad infecciosa pueden ser suficientes para constituir
un brote.
Traducción oficial/Official translation/Traduction officielle
3.12
epidemia
gran número de casos de una enfermedad infecciosa (3.9) en particular, que ocurren al mismo tiempo en
una comunidad o región geográfica
[FUENTE: ISO 28901:2011, 3.6, modificada — se agregó "infecciosa" después de "enfermedad", se
eliminó "normalmente infecciosa", se reemplazó "comunidad en particular" por "comunidad o región
geográfica" en la definición.]
3.13
pandemia
propagación mundial de una enfermedad infecciosa (3.9)
Nota 1 a la entrada: Una pandemia es declarada por la Organización Mundial de la Salud (OMS).
[FUENTE: ISO/PAS 45005:2020, 3.5, modificada — se agregó "infecciosa" después de "enfermedad" y se
agregó la Nota 1 a la entrada.]
3.14
enfermedad infecciosa endémica
enfermedad infecciosa (3.9) ya sea constantemente presente o habitualmente prevalente en una región
geográfica concreta
4 Contexto de la organización
4.1 Generalidades
La organización debería obtener y tomar conciencia sobre enfermedades infecciosas conocidas
y emergentes que pueden, o es probable que afecten significativamente, a la organización o sus
actividades.
La organización debería determinar las cuestiones externas e internas y considerar:
a) los peligros específicos y los riesgos relacionados con enfermedades infecciosas para los
trabajadores y otras partes interesadas que pueden verse afectados por las actividades de la
organización (por ejemplo, visitantes, clientes, usuarios de servicios, público) (véanse 8.1, 8.2 y
8.3);
b) si se debieran realizar cambios en sus operaciones para abordar los riesgos (véase 8.4);
c) cómo los trabajadores pueden ser apoyados para trabajar de manera segura (véanse los Capítulos 11
a 17).
NOTA 1 Las enfermedades infecciosas pueden variar en ocurrencia, impacto y gravedad según el país o la
región.
NOTA 2 Los controles apropiados pueden variar según el país o la región.
4.2 Cuestiones externas
Al determinar cuestiones externas, la organización debería considerar:
a) aparición y/o prevalencia de enfermedades infecciosas dentro de la comunidad local (incluso en
otras organizaciones y otros lugares de trabajo);
b) circunstancias locales, regionales, nacionales e internacionales y los requisitos legales y otros
requisitos relacionados, y orientación (por ejemplo, probabilidad de que las enfermedades
infecciosas sean transmitidas a través de personas, productos o servicios que se mueven de un
lugar a otro);
Traducción oficial/Official translation/Traduction officielle
c) disponibilidad de los servicios clínicos, las pruebas, los tratamientos y las vacunas;
d) disponibilidad de suministros de seguridad, salud y otros (por ejemplo, EPP, protectores faciales,
higienizantes de manos, termómetros, materiales de limpieza y desinfección);
e) posibles cambios o problemas en la cadena de suministro;
f) los modos de transporte que utilizan los trabajadores para ir y volver del trabajo (por ejemplo,
transporte público, automóvil, bicicleta, caminar, transporte compartido);
g) trabajadores que viajan a regiones con una enfermedad infecciosa endémica o con un brote de una
enfermedad infecciosa;
h) el acceso de los trabajadores a servicios de guardería y educación para sus niños;
i) idoneidad del hogar del trabajador para el trabajo a distancia;
j) situaciones domésticas de los trabajadores (por ejemplo, vivir con alguien que tiene un mayor
riesgo de contraer una enfermedad infecciosa o desarrollar enfermedades graves a causa de
enfermedades infecciosas);
k) la continuidad de los servicios esenciales (por ejemplo, provisión de alimentos, infraestructura
doméstica, servicios públicos);
l) cambios en las necesidades y expectativas, o en el comportamiento de las partes interesadas
pertinentes;
m) la cultura local y los comportamientos culturales (por ejemplo, besarse, abrazarse, estrechar la
mano);
n) aumento o disminución de la demanda de los productos/servicios de la organización.
4.3 Cuestiones internas
4.3.1 Generalidades
Al determinar las cuestiones internas, la organización debería considerar:
a) prevalencia o probabilidad de una enfermedad infecciosa en la organización;
b) fuentes de agentes infecciosos en el lugar de trabajo que pueden provocar una enfermedad
infecciosa;
c) capacidad de la organización para adquirir conocimientos actualizados sobre enfermedades
infecciosas;
d) el tipo de organización y actividades relacionadas (por ejemplo, producción primaria, procesamiento,
fabricación, servicios, venta minorista, asistencia social, formación u otra educación, reparto o
distribución);
e) número, ubicación y tipos de lugares de trabajo potencialmente afectados (por ejemplo, oficinas,
fábricas, talleres, almacenes, plantas de tratamiento de agua, vehículos, puntos de venta minorista,
hogares propios de los trabajadores u hogares de otras personas);
f) como se organiza el trabajo (por ejemplo, cambios en las exigencias del trabajo, el ritmo de trabajo,
la presión del tiempo, el trabajo por turnos, los requisitos de desplazamiento) y cómo esto impacta
en la seguridad, la salud y el bienestar de los trabajadores;
g) disponibilidad de recursos (por ejemplo, operativos, de seguridad y salud, higiene);
h) valores culturales dentro de la organización que pueden afectar a los controles de riesgos;
Traducción oficial/Official translation/Traduction officielle
i) la relación entre los trabajadores y la organización (por ejemplo, empleados, contratistas,
voluntarios, trabajador independiente, a tiempo parcial, trabajadores por turnos, trabajadores a
distancia);
j) necesidades específicas de los trabajadores que se considera de alto riesgo de contraer una
enfermedad infecciosa o desarrollar enfermedades graves a causa de enfermedades infecciosas
(por ejemplo, trabajadores con problemas de salud subyacentes);
k) necesidades específicas derivada de la diversidad de trabajadores (véase 4.3.2);
l) barreras lingüísticas y cuestiones de comunicación;
m) el grado en que es posible implementar controles de infección específicos en un lugar de trabajo o
en relación con actividades de trabajo o con maneras de trabajar;
n) el aumento de ausencias de los trabajadores (por ejemplo, debido a enfermedad, requisitos de
cuarentena o autoaislamiento, duelo).
4.3.2 Diversidad de trabajadores y otras partes interesadas pertinentes
La organización debería tener en cuenta toda la diversidad de sus trabajadores y otras partes
interesadas pertinentes al determinar cuestiones internas (véase 4.3.1) en relación con la prevención
y la gestión de enfermedades infecciosas. La organización debería considerar que cada trabajador y
otras partes interesadas pertinentes tienen necesidades diferentes, basadas en sus características y
circunstancias personales, tales como:
a) necesidades específicas de género;
b) embarazo o parto reciente;
c) aquellos que cuidan o viven con personas vulnerables (por ejemplo, bebés, miembros de la familia
inmunocomprometidos);
d) edad, teniendo en cuenta tanto a los trabajadores mayores como a los más jóvenes;
e) discapacidades;
f) etnia, cultura y fe;
g) aquellos con problemas de salud subyacentes (por ejemplo, inmunocomprometidos, asmáticos).
NOTA 1 Las discapacidades pueden afectar a la idoneidad de los controles de enfermedades infecciosas,
incluida la accesibilidad a edificios, instalaciones, equipos o servicios. Las discapacidades incluyen limitaciones
físicas y mentales. Las personas con discapacidad pueden incluir usuarios de sillas de ruedas, personas con
limitación motriz, auditiva o visual, o con un problema o enfermedad que tenga un impacto en su capacidad
mental.
NOTA 2 Muchas personas tienen discapacidades o vulnerabilidades a enfermedades infecciosas, o necesidades
específicas que no son evidentes de inmediato (por ejemplo, personas con diabetes, problemas respiratorios,
problemas cardíacos, limitación auditiva).
5 Características de las enfermedades infecciosas
Como parte de la evaluación de riesgos, la organización debería tener en cuenta las características de las
enfermedades infecciosas que probablemente impacten a los trabajadores y otras partes interesadas,
de modo que se puedan determinar los controles adecuados (véase el Capítulo 8). Las características de
una enfermedad infecciosa incluyen:
a) virulencia del agente infeccioso que causa la enfermedad;
b) probabilidad de transmisión;
Traducción oficial/Official translation/Traduction officielle
c) periodo de incubación;
d) periodo de tiempo durante el cual las personas pueden transmitir una enfermedad contagiosa;
e) extensión de tiempo que un agente infeccioso permanece infeccioso en objetos o materiales
contaminados;
f) síntomas relacionados con la enfermedad infecciosa;
g) gravedad potencial de las enfermedades (véase la Tabla A.1);
h) fuentes y modos de transmisión, incluidos:
1) un agente infeccioso transportado por otra persona que se transmite a través del contacto
piel a piel, desechos biológicos o intercambio de fluidos corporales (por ejemplo, riesgos del
cuidado personal, interacción sexual);
2) animales o insectos que están infectados o son portadores de un agente infeccioso (por ejemplo,
a través del tacto, picaduras o mordeduras);
3) fuentes ambientales contaminadas (por ejemplo, a través del agua o el aire);
4) inhalación (por ejemplo, esporas de moho, inhalación de fluidos corporales al toser);
5) ingestión (por ejemplo, al comer alimentos contaminados);
6) punción de la piel (por ejemplo, inyecciones, heridas);
7) contacto con una superficie u objeto contaminado (por ejemplo, agujas usadas, manijas de
puertas).
La organización debería buscar asesoramiento de:
— organismos de confianza (por ejemplo, autoridades de salud pública, centros de control de
enfermedades, la Organización Mundial de la Salud, la Organización Internacional del Trabajo);
— especialistas (por ejemplo, epidemiólogos, médicos especializados en enfermedades infecciosas,
higienistas y especialistas en salud en el trabajo, profesionales de la salud pública y otros expertos
en enfermedades infecciosas).
La organización debería ser consciente de que la información sobre enfermedades emergentes cambia
con el tiempo.
NOTA Algunas personas infectadas no presentan síntomas, pero pueden transmitir la enfermedad.
6 Liderazgo y participación de los trabajadores
6.1 Liderazgo
La alta dirección y los gerentes de todos los niveles deberían demostrar liderazgo para gestionar
eficazmente los riesgos para los trabajadores y otras partes interesadas pertinentes derivados de
enfermedades infecciosas que existen, o que pueden existir, en el lugar de trabajo.
La alta dirección debería comunicar a los trabajadores y otras partes interesadas:
— cómo deberían ser notificadas las preocupaciones o la incidencia de las enfermedades infecciosas;
— el compromiso de la organización con la transparencia en la gestión de enfermedades infecciosas;
— acciones a tomar si una persona ha contraído o sospecha que ha contraído una enfermedad infecciosa;
Traducción oficial/Official translation/Traduction officielle
— acciones que la organización tomará para apoyar a los trabajadores y otras partes interesadas
pertinentes cuando haya un brote de una enfermedad infecciosa o un incidente de enfermedad
infecciosa;
— apoyo a los trabajadores para que se retiren de situaciones del trabajo que se cree que presentan un
riesgo inminente o grave para la vida o la salud.
Cuando se conoce que una enfermedad infecciosa es, o puede ser, un problema, la alta dirección debería:
a) proporcionar recursos adecuados (véase el Capítulo 10) y ponerlos a disposición de manera
oportuna y eficaz;
b) consultar y fomentar la participación de los trabajadores y de los representantes de los trabajadores,
cuando existan, en la toma de decisiones que afectan a la seguridad, la salud y el bienestar
relacionados con el trabajo (véase 6.2);
c) proporcionar apoyo adecuado a los trabajadores que no pueden trabajar, incluida la provisión de
una baja adecuada del trabajo, remunerada si es posible (pa
...






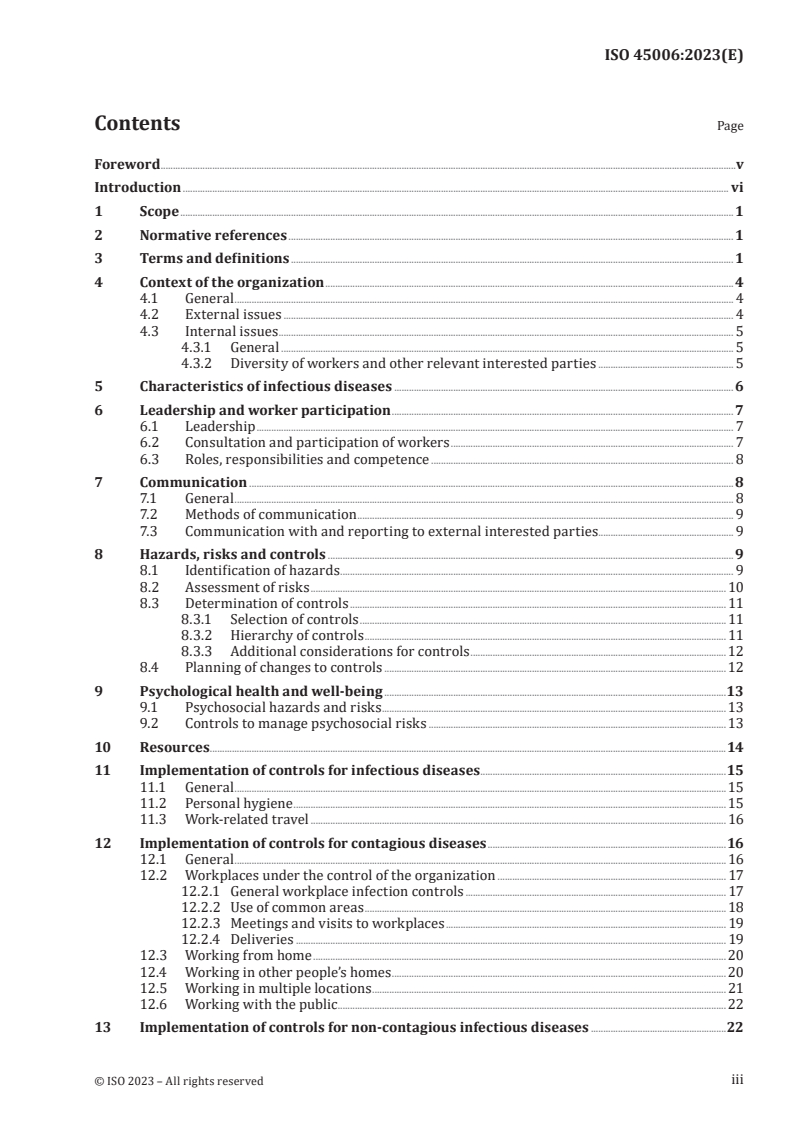

Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.
Loading comments...